Thirty-three: that’s how many joints are in just one foot. Each of your feet also contains 26 bones, plus a whole lot of muscles, tendons, and ligaments — making them a prime target for rheumatoid arthritis. Rheumatoid arthritis (RA) is a chronic, inflammatory disorder in which your immune system mistakenly attacks the lining of membrane that surrounds your joints. It tends to target smaller joints first, such as those in your hands — and often, your feet. In fact, more than 90 percent of people with RA will develop pain, stiffness, swelling or other symptoms in the foot and ankle over the course of the disease, according to the American Academy of Orthopaedic Surgeons. You can read here about common rheumatoid arthritis symptoms.
How Rheumatoid Arthritis Affects the Feet
Joints are covered with a lining called synovium. Its job is to lubricate the joint so it moves more easily. RA causes an overactivity in this lining. The synovium becomes inflamed, thickens, and produces an excess of joint fluid. That extra fluid — along with the inflammatory chemicals released by the immune system — causes swelling, damages cartilage and softens the bone within the joint. A systemic disease, RA also affects ligaments and surrounding soft tissue, says Brett Sachs, DPM, foot and ankle surgeon in Colorado. “When that happens, the joints start to weaken and that’s when the deformities can occur,” explains Dr. Sachs, who is also a fellow member of the American College of Foot and Ankle Surgeons. Rheumatoid arthritis tends to affect the joints in your feet more quickly in part because they are smaller, says Dr. Sachs. Research shows in about 20 percent of RA patients, foot and ankle symptoms are the first signs of the disease.
What Does Rheumatoid Arthritis in the Feet Feel Like?
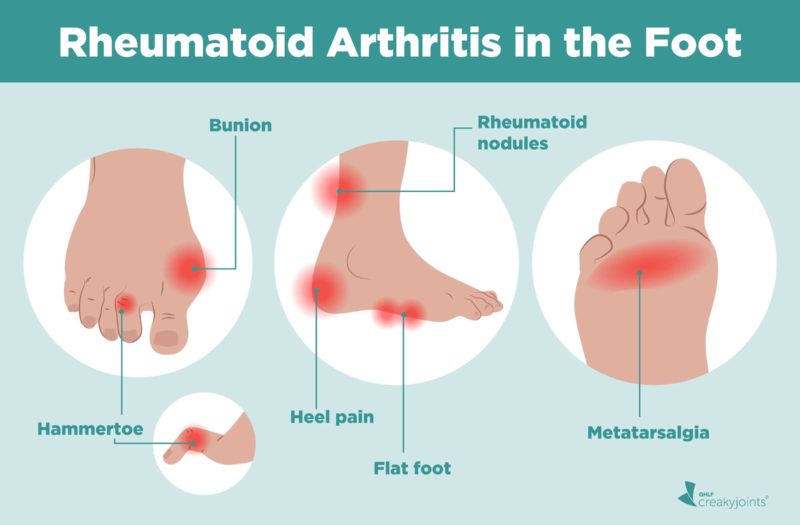
When your feet are affected by rheumatoid arthritis, you may experience swelling, redness, and a feeling of warmth around the affected joints. Pain is very common as well. In one study comparing foot problems in RA patients versus people without arthritis, 98 percent of RA patients had foot pain and 96 percent reported some difficulty in function, compared to 76 percent and 66 percent, respectively, in the healthy group. Compared with osteoarthritis, which typically affects one specific joint, rheumatoid arthritis usually occurs in the same joints on both sides of your body — so it commonly affects both feet at once. Symptoms may flare, then go into periods of remission. Here’s more information about coping with rheumatoid arthritis flares. Over time, rheumatoid arthritis can cause joints to deform and shift out of place. Specific foot problems caused by RA include:
Pain across the ball of your foot
The medical term is metatarsalgia — and it’s the most common foot issue associated with RA, says Jonathan Rouse, DPM, a podiatrist based in Nebraska and spokesperson with the American Podiatric Medical Association. Once the intrinsic (or deeper) muscles in your foot lose their stabilizing forces, dislocations or deformities can occur at the metatarsophalangeal joint (which connects the toe to the foot), thus increasing pressure on the forefoot and causing pain and inflammation across the ball of the foot, explains Dr. Rouse. People with RA may also experience fat pad atrophy — or a thinning and wearing out of the normal fat pad that goes across the ball of your foot — which can exacerbate pain, adds Dr. Sachs.
Bunion
This hard, painful, bony lump that forms on the joint at the base of your big toe is a common complaint among RA patients, says Dr. Sachs. It occurs when some of the bones in the front part of your foot move out of place, causing the big toe to push against the next toe and the joint at the base of your big toe to stick out, according to the Mayo Clinic. Sometimes your big toe turns so far in that it moves on top of the toe next to it.
Hammertoe and claw toe
Weakened ligaments from RA can cause these two joint deformities, conditions where toes are permanently bent and curled under, like a claw. Hammertoe in the second toe is common in people who have a bunion in the big toe.
Heel pain
As RA progresses, the hindfoot (or heel region) will begin to lose stability, says Dr. Rouse. The plantar fascia — a ligament that connects the heel to the front of the foot — will still try to do its job and support the arch of your foot, he explains; however, the added stress and inflammation will weaken the structure and can lead to pain.
Changes in the shape of your foot
Flatfoot deformity — a progressive flattening of the arch of your foot — can occur in rheumatoid arthritis, when tendons, ligaments, and bones shift out of their normal positions, causing pain and discomfort along inside or outside of your ankle. If RA damages ligaments that support the top of your foot, your arch may also collapse, which can cause the front of the foot to point outward, according to the American Academy of Orthopaedic Surgeons. Shape changes in the front of the foot and toes can create pressure sites that then develop calluses, or areas of hard thickened skin. All of these changes in the shape of the foot can make it very difficult to comfortably wear shoes.
Rheumatoid nodules
Some people with RA develop hard lumps under the skin called nodules, often around pressure points. In the feet, nodules may appear over the Achilles tendon, in the heel pad or over any bony spots, and can cause pain if they rub against shoes or along the floor while you walk.
How to Keep Your Feet Healthy with Rheumatoid Arthritis
Though there is no cure for rheumatoid arthritis, you can take steps to manage symptoms and stay active. To help keep your feet healthy:
1. Stick to your RA treatment plan
This is key to ease symptoms and reduce the risk of deformity, says Dr. Sachs. Depending on the severity of your symptoms and how long you’ve had rheumatoid arthritis, your rheumatologist may prescribe a combination of medications. The goal of RA treatment is to stop systemic inflammation so you can achieve low disease activity or remission, which can prevent symptoms like pain and fatigue, as well as long-term joint and organ damage. Commonly prescribed medications include non-steroidal anti-inflammatory drugs (NSAIDs) to relieve pain and reduce inflammation, steroids to reduce inflammation and slow joint damage, disease-modifying antirheumatic drugs (DMARDs) to slow the progression of RA, or biologics, which are more complex, targeted DMARDs that act on certain immune system pathways that trigger inflammation.
2. Exercise
It may seem counterintuitive, but staying active can help ease arthritis symptoms in your feet, says Dr. Sachs. Here’s why: Regular exercise and stretching strengthens muscles, keeps joints flexible, and reduces pain in alljoints — from your hips and shoulders to your ankles and feet. Plus, it helps burn calories, so you shed extra pounds and lighten the load on the joints of your feet. It’s important to find comfortable ways to stays active if you have foot pain. Low-impact exercise that doesn’t cause you to bear as much weight on your feet (think swimming or biking) is less stressful on the joints in your feet. Here are daily stretches you can try for arthritis foot pain. Talk to your doctor or podiatrist about which of these and other moves are safe for you.
3. Rest through RA flares
“They can come out of nowhere,” says Dr. Rouse. His advice: “Rest as much as possible to let the inflammatory process dissipate before becoming active again.” Ice or other forms of cold therapy can also help reduce swelling and pain during flare of RA. Here are more tips to help handle arthritis flare-ups.
4. Make sure the shape of your shoes matches the shape of your feet
That may mean a roomy toe box to accommodate bunions or hammertoes, or an extra-wide shoe to reduce pressure on painful spots. Sturdy, supportive shoes are crucial to ease arthritis foot pain. Custom orthotics or a good over-the-counter shoe insert can provide even more comfort and extra support, adds Dr. Sachs. “These inserts can help rebalance the foot, give your arch more support, and help cushion the ball of your foot.” Talk to your doctor to determine the best footwear for you. Here are more tips for picking the right shoes when you have arthritis.
5. Consider a steroid shot
Cortisone injections into the affected joint can help reduce inflammation. The catch: It’s a temporary fix, and it won’t stop the progression of the disease.
6. Schedule a surgery consult
Depending on how much cartilage damage you have and your response to other RA treatments, your doctor may recommend foot surgery. Fusion of the affected joints is the most common type performed for RA, according to the American Academy of Orthopaedic Surgeons. The procedure takes the two bones that form a joint and fuses them together to make one bone. Other types of surgery can help correct bunions or hammertoes in some patients. Your doctor will determine your best course of treatment.
Not Sure What’s Causing Your Foot Pain?
Check out PainSpot, our pain locator tool. Answer a few simple questions about what hurts and discover possible conditions that could be causing it. Start your PainSpot quiz.
If you enjoyed reading this article, you’ll love what our video has to offer.
de Andrade AP, et al. Foot function in rheumatoid arthritis patients: a cross-sectional study. Clinical Rheumatology. July 2018. doi: https://doi.org/10.1007/s10067-018-4215-y. Interview with Brett Sachs, DPM, foot and ankle surgeon in Colorado Interview with Jonathan Rouse, DPM, a podiatrist based in Nebraska and spokesperson with the American Podiatric Medical Association Hammertoe. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/hammertoe-and-mallet-toe/multimedia/hammertoe/img-20005966. Jaakkola JI, et al. A Review of Rheumatoid Arthritis Affecting the Foot and Ankle. Foot and Ankle International. December 2004. Doi: https://doi.org/10.1177/107110070402501205. Metatarsalgia. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/metatarsalgia/symptoms-causes/syc-20354790. Rheumatoid arthritis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648. Rheumatoid Arthritis in the Foot and Ankle. Foot Health Facts. American College of Foot and Ankle Surgeons.https://www.foothealthfacts.org/conditions/rheumatoid-arthritis-in-the-foot-and-ankle. Rheumatoid Arthritis of the Foot and Ankle. OrthoInfo. American Academy of Orthopaedic Surgeons.https://orthoinfo.aaos.org/en/diseases–conditions/rheumatoid-arthritis-of-the-foot-and-ankle.