“Burnout has opened space to look at who I am outside of advocacy. It has made room for me to discover what I want this next part of my life to look like. I’m learning to see this as an opportunity and not a failure.”
Still Wearing a Mask
“Masking is absolutely a matter of life or death for me. But I am not ashamed, and I will not be afraid to take care of myself…It is a part of me.”
A Guide to Setting Boundaries if You’re a People-Pleaser
Saying no isn’t always easy, but with practice, it can become a habit.
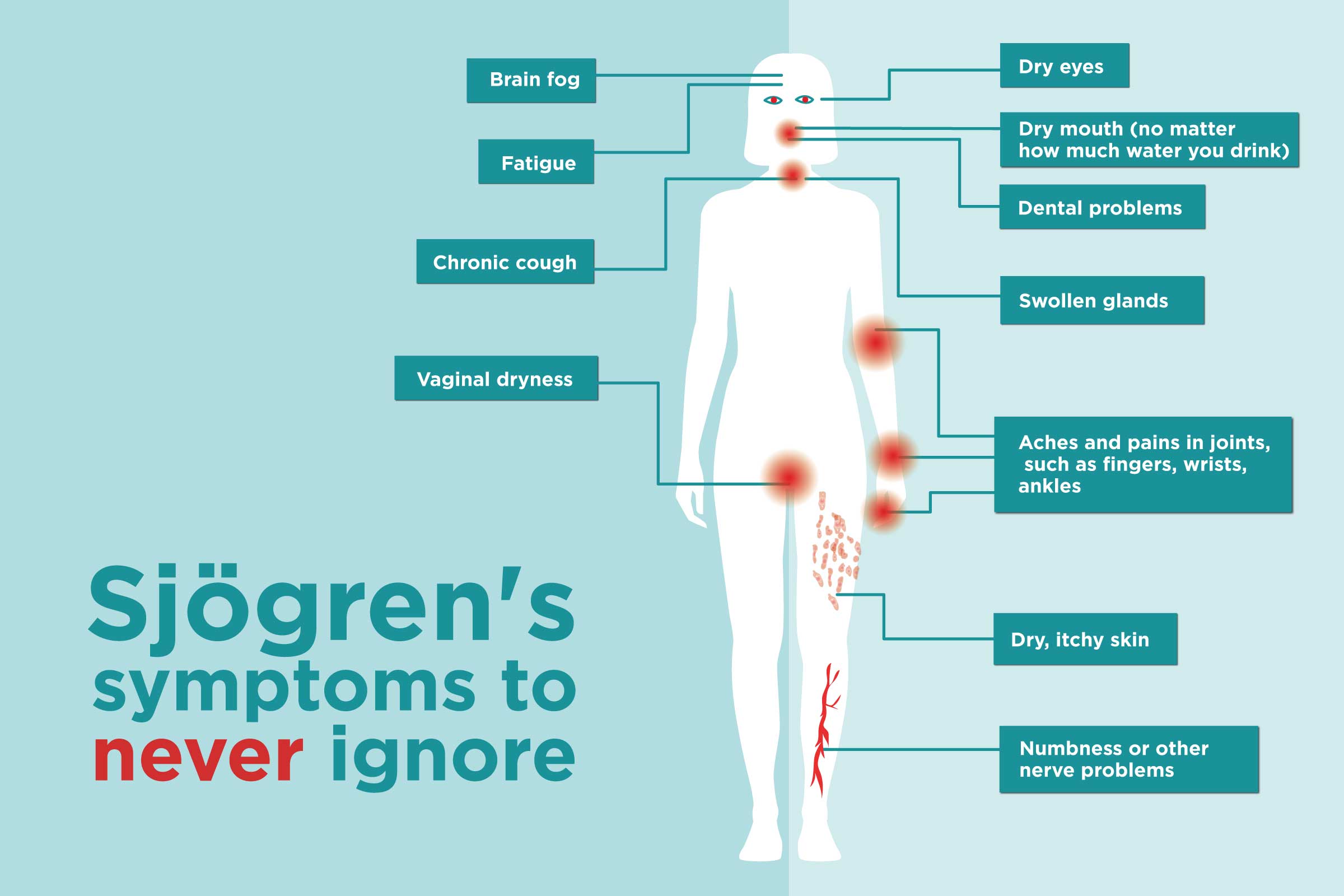
Thanks to high-profile voices like Venus Williams and Halsey, more people are hearing about Sjögren’s disease. Now let’s make sure what they hear is accurate — because Sjögren’s is a serious systemic disease, and the science behind it is moving fast.
10 December Health Tips for People Living with Chronic Illness
From early prescription refills to masking in crowds and planning for flares, here are essential steps to stay healthy and prepared for December with a chronic condition.
Understanding Neuromodulation and Vagus Nerve Stimulation: A New Way to Treat Rheumatoid Arthritis
Vagus nerve stimulation and splenic nerve stimulation are being studied for their potential to help RA patients who don't respond to medication such as biologics. Here’s what you need to know.
Patient advocate Shelley Fritz shares her experience with PRP therapy and why it was the best choice for her hand osteoarthritis.
I Experienced Immune-Related Adverse Events — While Having Cancer and an Autoimmune Disease
"Trying to balance turning on your immune system to fight your cancer — but not making your life more difficult as a result — is a hard thing to do. The doctors don't have all the absolute right answers and neither does anybody else. However, if you’re able to say what you’re feeling and what you think you need, that’s really important."
Donna’s IgG4-Related Disease Diagnosis Journey: A Roller Coaster of Emotions
She remained asymptomatic for IgG4-RD until the silent disease brewing inside her led to the unexpected loss of a kidney.
A new update recommended by the FDA would target the most transmissible variant so far, subvariant XBB.1.5.
Travel Pains and COVID-19 — How to Decide if You’re Ready to Travel This Summer
If you’re tired of being cooped up but are nervous about jet setting, here are a few key things to consider.
Why the COVID-19 Virus Keeps Mutating — and What It Means for You
A new COVID-19 variant isn’t immediately a cause for concern, but here’s how to know when it’s time to be extra vigilant.
Struggling to get an appointment with a doctor? Discover why this is happening and what you can do to get in sooner.
Recession-Proofing Your Health Care
Living with chronic illness is costly, so when the economy looks bleak it's natural to feel anxious about health care expenses. Here's help.
Everything You Need to Know If You’re Prescribed Paxlovid as an Immunocompromised Patient
See answers to all of your questions about this antiviral pill — from how it works to side effects and more.
Why Patients Speaking at National Conferences Matters
How a Nobel Prize Discovery Gives New Hope for Calming the Immune System in Autoimmune Diseases
The Global Healthy Living Foundation (GHLF) celebrates the 2025 Nobel Prize in Physiology or Medicine, awarded to three scientists—Shimon Sakaguchi, Mary Brunkow, and Fred Ramsdell—for a groundbreaking discovery about how our immune system works.
Patient-Friendly News You Can Use: Special American College of Rheumatology Edition
The latest health headlines to help you stay informed, take control of your care, and advocate for better health.
A well-intentioned drug pricing reform under the Inflation Reduction Act (IRA) could lead to higher out-of-pocket costs and serious health risks for Medicare patients—despite its goal to lower drug prices.
Want to Have a More Successful Rheumatologist Visit? Try These 25 Tips from CreakyJoints Members
Here’s what to do before, during, and after a doctor visit to get better care and treatment.
Invisible Illness Patients: You May Need to Dress for Doctor Visits to Match How You Physically Feel
The best advice arthritis patient Nicole Dalton ever received: "You have to dress to match how you physically feel."