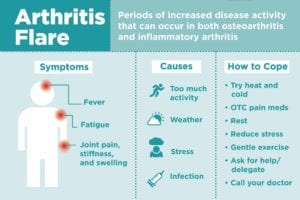
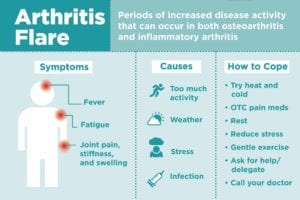
You’re feeling good, barely thinking about your chronic pain, and then wham — an arthritis flare hits you like a Mack truck. These periods of increased disease activity take a toll on you physically and emotionally, especially because they can come on unexpectedly. If you’ve got either osteoarthritis or an inflammatory type of arthritis like rheumatoid arthritis, you probably know what we’re talking about.
So how can you deal with an arthritis flare-up when it happens? “I remind myself, ‘This, too, shall pass,’” arthritis patient Beth Bloomfield told us on Facebook. “Like a kidney stone!” another patient, Katie Resnick, joked back. Although arthritis flares are never pleasant, there are techniques that can help shorten their duration. Also important: Being able recognize when a flare is starting and avoid the triggers that may cause your flare-ups in the first place.
Symptoms of an Arthritis Flare
Joint pain
Osteoarthritis patients experience “joint pain, stiffness mostly associated with weather changes such as pressure change or cold, but usually no joint swelling,” says rheumatologist Nilanjana Bose, MD, an assistant professor at the University of Texas Medical Branch (UTMB) and a member of the American College of Rheumatology. Rheumatoid arthritis patients also experience joint pain and stiffness, as well as swelling.
Fatigue
“Fatigue can occur in the setting of flare in inflammatory arthritis, but not usually in osteoarthritis unless pain during the night is interfering with sleep,” says Dalit Ashany, MD, a rheumatologist at Hospital for Special Surgery.
Fever
In RA, “joint swelling is also associated with systemic symptoms like low-grade fevers,” Dr. Bose says. “The inflammatory cascade gets activated, including [immune system proteins called] cytokines, which leads to joint pain, swelling, and occasional systemic symptoms in severe flares.”
Causes of Arthritis Flares
Too much activity
You’re feeling good, so you overdo it, and then you end up with an arthritis flare. “Osteoarthritis often flares after overexertion of the joint or joints that are involved,” Dr. Ashany says. With OA, “unexpected activity can stress out the joints and surrounding tissues and cause pain,” Dr. Bose says. Too much activity can also lead to a flare in inflammatory arthritis patients, she notes.

Weather
“Pressure changes and humidity may play a role in exacerbating joint pain,” Dr. Bose says. If you live in a dry, hot climate, you may be less prone to the impacts of weather on your arthritis. “Patients with all types of arthritis, OA or inflammatory, often state that their joints are achier or even flare in cold or humid weather, although there is not a body of scientific data about this,” Dr. Ashany says.
Medical causes
Infections, such as respiratory viruses, can lead to flares as they affect the immune system. Medications for inflammatory arthritis, such as corticosteroids and biologics, can also make patients more vulnerable to infection; yet a “decrease in medication, either because of a deliberate reduction or patient non-compliance, can lead to flare,” Dr. Ashany says.
Stress
Although the exact mechanisms are unknown, “stress can also induce flares,” Dr. Bose says. It’s possible that stress may lead to the production of more pro-inflammatory cytokines. Try these self-care tips to minimize stress and flares.
Food
“There is no proof that a specific food causes arthritis flares, however if an individual clearly sees a relationship between a certain food and flare, then that may be relevant for that particular individual,” says Dr. Ashany. Dr. Bose advises, “I always recommend patients to avoid red meat and refined carbohydrates, which can be pro-inflammatory. Gluten can cause flares for certain patients.” Arthritis patient Anita Marie Poupa told us on Facebook that she avoids sugar, alcohol, and caffeine. Try these tips to cut out excess sugar.
Diagnosis and Treatment for Arthritis Flares
If you think you’re going through a flare that hasn’t improved after a couple of days, call your rheumatologist or primary care doctor. They will want to monitor how you feel and may want to order imaging and blood tests to see what’s going on. They can also prescribe medications to get the flare under control.
Physical tests
“The physical examination is important for determining flares,” Dr. Ashany says. “The physician will examine the patient for number of tender and swollen joints. Having more than you did at a prior visit suggests a flare.” In inflammatory arthritis, she says it’s also important that patients let her know if their current symptoms are typical of their previous flares.
Lab tests
In inflammatory arthritis, “some patients will have an elevation of inflammatory markers, such as ESR and/or CRP, during a flare,” Dr. Ashany says. “Other labs that can be altered during a flare are platelets which can become elevated or the blood count which can show anemia.” In osteoarthritis, laboratory markers are not usually altered, Dr. Bose says. Read more about the ESR, or sedimentation rate, blood test.
Common medications to treat arthritis flares


OA patients might just need some OTC pain-relieving medication such as acetaminophen, ibuprofen, or naproxen. Dr. Bose also recommends topical gels and lotions like diclofenac gel or 2 Old Goats. If that doesn’t work, Dr. Ashany says joint injections of steroids may be given. RA flares are more complicated. “In inflammatory arthritis, steroids are often used to try to quickly bring a flare under control,” Dr. Ashany says. If only one joint is involved a steroid (such as depomedrol) can be given by injection, but otherwise it can be taken orally (such as prednisone).
In inflammatory arthritis, “if flares continue to occur, this indicates that the patient’s regimen of maintenance medication is not adequate,” Dr. Ashany says. “This may lead to addition of a medication, switching one drug for another or increasing the dose of medication that the patient is currently taking.”
Tips on Coping with Arthritis Flares
Prepare ahead of time
Keep track of when your flares happen so you can learn to identify triggers. If you think, for example, that weather affects your flares, OA patients “need to prepare accordingly and use OTC pain meds,” Dr. Bose says. In addition, RA patients should stay compliant with their medication regimen. If you suspect your diet could be a culprit, monitor what foods you’re eating, says Karen Jacobs, EdD, OT, OTR, CPE, FAOTA, an occupational therapist who works with arthritis patients and a clinical professor at Boston University.
Have a plan for when flares inevitably occur. Jacobs says to arrange ahead of time with your employer to work from home or make other adjustments if needed. “An inflammatory arthritis patient will often, in time, have a sense of whether they are starting to flare,” Dr. Ashany says.

Get your rest
If you feel like you just can’t get anything done, don’t. “Rest is critical,” Jacobs says. “It might be at this point you put on your arthritis gloves and take a nap.” All the patients we talked to agreed that rest is their go-to flare fighter. “Resting, curling up with a good book or finding some comedies to watch on TV,” Brenda Kleinsasser said of her routine. Here are inspiring books that can help you cope with chronic illness.
Reduce stress
Stress can cause arthritis flares — and arthritis flares can cause stress. Learn to recognize what you can handle emotionally. “I like to just shut myself away from the world as I need all my energy getting through it,” arthritis patient Karen Nash said on Facebook. “If there is anyone around, I feel I need to pretend I am better than I am and hold a conversation, which is just too much.”
Jacobs advises stress reduction and relaxation techniques like deep breathing and meditation. “App stores have lots of great meditation apps,” she says. Try Headspace, The Mindfulness App or Calm to see which one works for you. Aromatherapy may also help.
Try heat and cold
“You might use hot or cold packs,” Jacobs says. The patients we talked to on Facebook use different kinds of temperature treatments, including ice, warm baths or showers, heating pads, paraffin wax for feet and hands, heated blankets, and hot tubs. Here are different ways to try heat therapy and different ways to try cold therapy.
Distract yourself
Mental techniques come in here as well: If you focus on the pain, it’s just going to hurt more. “Rest followed by light routine so as not dwell on the pain,” arthritis patient Amanda Edwards said on FB. “Knowing what is mine to handle.” Alex Woodward also told us: “Distraction: pain meds, PJ’s, chocolate, and laptop to either research an interesting or weird subject, or plan a road trip.”
Gentle exercise
Jacobs says that very gentle hand exercises could help reduce inflammation. If you can handle it, some light movement may make you feel better mentally and physically. Check with your doctor to see if low-impact tai chi or yoga are right for you.
Ask for help
“A lot of times we want to be these warriors and won’t reach out for people to help us, but think about what else people can do,” Jacobs says. Others might not know what you’re going through, and want to pitch in. “Speak up and communicate with family, friends, and doctors,” arthritis patient Michelle Grabarek told us on Facebook.
Call your doctor
Speaking of doctors, you may or may not need to reach out. If your symptoms are mild and go away quickly, you probably don’t need to. But, “there is no way to predict if a mild flare is going to turn into a severe flare,” says Dr. Ashany, who notes that a swollen, warm, and red joint should always lead to an immediate phone call, “as patients can also potentially develop an infected joint, which needs to be treated immediately.” If you have any questions, play it safe and call your doctor. “If a flare occurs, please contact your doctor so you can start treatment promptly if needed,” Dr. Bose says.
Keep Reading
Subscribe to CreakyJoints
Receive our newsletter and stay informed about arthritis treatments, comorbidities, and more.





