On the surface, gout, a type of inflammatory arthritis caused by elevated levels of uric acid, may seem very straightforward — and sometimes it is. In the classic gout presentation (which is what most patients experience), gout pain goes from zero to 60 quickly, strikes in the middle of the night, and primarily affects the joint in the big toe.
But gout doesn’t always happen like that. About 25 percent of patients with gout feel pain in multiple joints, and the toe isn’t necessarily one of them. Here are other gout symptoms to be aware of.
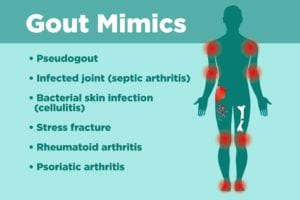
When your knees, wrists, and/or elbows are hurting, it’s not as easy for a doctor to conclude that gout is to blame. In fact, rheumatologists consider gout to be a “great imitator” because it has the potential to cause symptoms that closely mimic those of other conditions, says Joseph Huffstutter, MD, a rheumatologist with Arthritis Associates in Hixson, Tennessee. The problem, of course, is that when gout masquerades as something else it can end up delaying proper treatment.
If you’ve been diagnosed with one of the following conditions, your doctor might very well have gotten it right, but there’s a chance you actually have gout instead (or vice versa).
1. Pseudogout
It sounds like gout, it looks like gout, but it’s not gout. Confused? So are many people with pseudogout, formally known as calcium pyrophosphate (CPP) crystal deposition disease. Both conditions occur when crystals settle in one or more joints, leading to pain and inflammation. The difference comes down to what those crystals are made of. For gout, it’s uric acid. For pseudogout, it’s crystallized CPP.
If you have an acute case of gout, your doctor should be able to aspirate fluid from the affected joint, examine it under a microscope, and see needle-shaped crystals with sharp edges.
But if you’re not in the midst of a gout flare, it’s going to be harder to sort it out, says Kaitlin A. Quinn, MD, a rheumatologist at Medstar Georgetown University Hospital in Washington, D.C. Here’s more information about pseudogout symptoms and treatment.
2. Infected joint (septic arthritis)
A single joint that’s red, hot, and swollen might be gout — or it might be septic arthritis. To further add to the confusion, both conditions can cause you to develop a fever and for your white blood cell count to spike. In either instance, your body thinks you have an infection it’s trying to fight off, but in only one of those cases (septic arthritis) is an infection present.
If you actually have septic arthritis, lab analysis of fluid taken from the impacted joint should reveal the particular organism that’s causing an infection.
3. Bacterial skin infection (cellulitis)
You have a fever, chills, and an area of your skin — probably somewhere on a lower leg — is red and hot and painful to touch. It could be gout, or it could be cellulitis, which is a potentially serious infection that occurs when bacteria infiltrates your skin via a cut or crack.
Unfortunately, if your doctor thinks there’s a chance you might have cellulitis, trying to extract fluid to test it for possible gout is a really bad idea because it could cause the infection to spread further. But they might take blood and skin samples and use those to test for signs of bacteria like strep or staph that tend to cause cellulitis.
4. Stress fracture
If you broke your toe, you would know it, right? While you’d certainly be able to connect the dots if you dropped a heavy object on your foot and the pain started right after, sometimes the origin of toe pain isn’t so clear. If your doctor suspects that you might have a fractured your toe (or any other joint), an X-ray might be in order.
5. Rheumatoid arthritis
Gout is often confused with rheumatoid arthritis (RA), says Dr. Huffstutter, especially in patients who have polyarticular gout, which means that gout impacts several joints. Both RA and gout can cause visible nodules, especially in the advanced stages. If you have gout, the bumps, which are called tophi, are made of lumps of uric acid crystals. No one really knows what causes nodules to form in people with RA, but about 25 of RA patients end up getting them. Here’s more about rheumatoid nodules and more information about gout tophi.
To figure out whether you might have gout or rheumatoid arthritis, your doctor might order a number of blood tests that, when positive or high, are associated with RA. Those include anti-CCP, C-reactive protein, erythrocyte sedimentation rate, and rheumatoid factor. Your doctor might also test joint fluid from one of your nodules to see if it contains uric acid crystals, which would point to gout.
6. Psoriatic arthritis
As with RA, psoriatic arthritis (PsA) sometimes causes swelling around the fingers or toes that can look a lot like gout tophi. The swelling in PsA is called dactylitis, and it gives digits a sausage-like appearance. If you have PsA, you might also have skin plaques that are indicative of psoriasis. (While you can have PsA without skin psoriasis, the conditions often go together.) Many people with PsA also have pitted fingernails, which is not something that should happen if you have gout.
And, of course, if you have PsA your doctor won’t find uric acid crystals in your joint fluid as they would if you had gout.
Keep Reading
If you enjoyed reading this article, you’ll love what our video has to offer.





