Treatment options for rheumatoid arthritis (RA), a chronic inflammatory disease that causes pain, stiffness, swelling, and loss of function in joints, have expanded dramatically over the past few decades. At the same time, doctors and researchers continue to gain new knowledge about the safety and efficacy of these available treatment options.
How can health care providers stay up to date and ensure that patients are getting the best available care? That’s where the American College of Rheumatology (ACR) treatment guidelines, which are updated every five years, can provide some direction.
The latest version of the guidelines, which was released this month and published in the journal Arthritis Care & Research, is based on a comprehensive literature review of high-quality research as well as the opinions of a voting panel comprised of 13 leading rheumatologists and two patient representatives. The goal of the guidelines is to provide current, science-backed advice on how to best manage this inflammatory disease.
Although these guidelines are primarily aimed at helping doctors make informed decisions about patient treatment, they are also beneficial for people with RA to know about.
“Being aware of the ACR guidelines gives patients more information, allowing them to be more informed and involved in the shared decision-making process,” says Shilpa Venkatachalam, PhD, MPH, Associate Director of Patient-Centered Research at the Global Healthy Living Foundation. Dr. Venkatachalam, who has rheumatoid arthritis, served as one of the patient representatives on the panel that created the 2021 ACR guidelines.
Keep in mind that the recommendations in these guidelines are a tool and not the final word on what will work best for you. Individual treatment decisions should always include input from patients and providers and take a variety of factors (including patient preferences and possible comorbid conditions) into account.
Also, the guidelines focus only on medication therapies to treat rheumatoid arthritis; they do not address “non-pharmacologic” approaches (such as exercise, diet, and stress management). This area will be covered in future guidelines, as will vaccines.
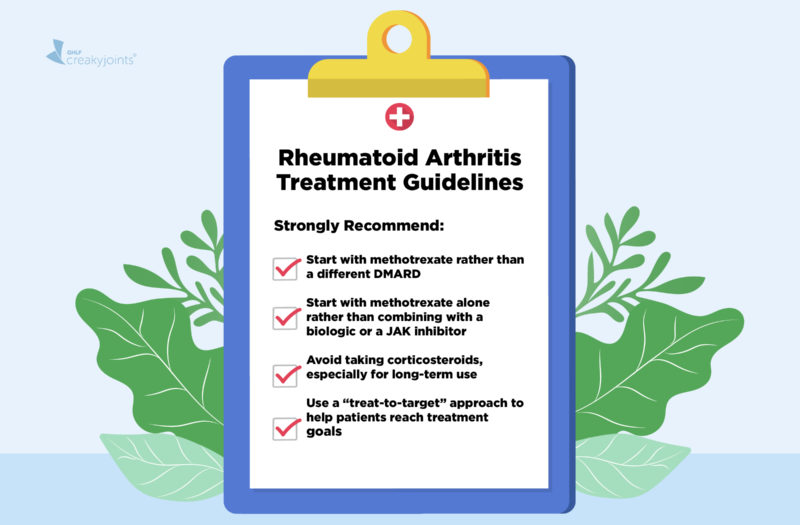
The 2021 guidelines reaffirm the disease-modifying antirheumatic drug methotrexate as the first-line treatment for RA and suggest avoiding glucocorticoids (corticosteroids, or steroids), as much as possible. In total, the guidelines feature 44 recommendations, but only seven are considered strong recommendations supported by ample evidence and/or high consensus among panel members.
It is commendable that the guidelines are notably influenced by patient preferences expressed in the voting panel, acknowledging throughout that there are many nuanced reasons patients may opt for certain treatment choices over others. This should allow doctors and patients to have better communication when it comes to shared decision-making, or deciding together what course of treatment is right for a given patient.
Strong Recommendations
The panel is highly confident that the benefits of these recommendations outweigh the risks for the majority of patients, due to moderate or high levels of evidence.
Newly diagnosed RA patients with moderate-to-high disease activity should start with methotrexate rather than other DMARDs like hydroxychloroquine or sulfasalazine. (For patients with low disease activity, the guidelines conditionally recommend hydroxychloroquine over other DMARDs as a first treatment, noting that it is better tolerated and has a more favorable risk profile.)
Newly diagnosed patients with moderate-to-high disease activity should take methotrexate alone rather than first opting for a biologic or small molecule drug (like a JAK inhibitor). Methotrexate alone is also preferable to a combination of methotrexate plus a biologic or small molecule drug for these patients.
Newly diagnosed patients should not take glucocorticoids for prolonged use (more than three months) when starting a conventional DMARD. Although the guidelines would prefer that patients begin DMARDs without needing to use any corticosteroids, they acknowledge that short-term (less than three months) use is sometimes needed to help alleviate pain and inflammation as a DMARD takes time to start working. The panel does, however, strongly recommend against using steroid medication over longer periods of time.
Patients who haven’t been previously treated with a biologic or small molecule drug should be managed using a “treat-to-target” approach. Treat-to-target entails frequent monitoring and tweaking regimens in order to get a patient to a predetermined goal, such as low disease activity. This may mean continuing to optimize the patient’s methotrexate dose or adding additional DMARDs if necessary.
Treat to target, however, is conditionally recommended for patients who have already had poor responses to biologics or JAK inhibitors. This is because there may be other factors that are affecting patients’ ability to hit a treatment target, such as the number of remaining available treatment options, the impact of non-inflammatory causes of pain, and patients’ threshold for continuing to change medications. In such cases, using shared decision-making to decide whether or when to change treatment may be preferred.
Patients starting a biologic, small molecule drug, or rituximab for the first time who have previously had hepatitis B (hepatitis B core antibody positive) should take antiviral drugs as a preventive measure instead of having their viral load and liver enzymes frequently monitored.
Conditional Recommendations
The panel is less confident that the benefits of these recommendations outweigh the risk, due to low certainty in the supporting evidence or because of substantial variation in patient preferences.
There are 37 conditional recommendations in the updated ACR guidelines. Although current guidelines are not directly compared to previous guidelines, there are a few notable changes from the 2015 guidelines.
Avoid using low-dose prednisone as bridge therapy.
This recommendation is a bit controversial. “It is recognized that many patients will require prednisone to help manage symptoms until DMARDs kick in. However, because of the toxicity associated with even low doses of prednisone — and the common finding that patients remain on low-dose prednisone much longer than originally planned when using as bridge therapy — the panel’s recommendation was to recommend against [it],” Liana Fraenkel, MD, MPH, adjunct professor of rheumatology at Yale School of Medicine and lead author of the new ACR guidelines, explained via email. “It is meant to ensure that rheumatologists do not default to using bridge therapy but only use it when absolutely necessary.”
Patients who don’t fare well enough on methotrexate alone should add a biologic or a targeted therapy (JAK inhibitor) instead of adding sulfasalazine and hydroxychloroquine to their regimen.
This is modified from the 2015 guidelines, which recommended triple therapy (a combination of methotrexate, sulfasalazine, and hydroxychloroquine). The main reason for this change was that the patient panel “strongly prioritized maximizing improvement as soon as possible.” The guidelines also acknowledge that there may be better persistence — patients may be able to better tolerate and stay on the medication regimen longer — by adding a biologic or JAK to methotrexate over starting triple therapy.
To make it easier to stay on methotrexate alone, the current guidelines also include advice about how to minimize methotrexate side effects. These tips (also a conditional recommendation) include splitting the dose of oral methotrexate over a 24-hour period, taking weekly subcutaneous injections instead of oral methotrexate, or taking extra folic acid.
The guidelines do not recommend a specific class of biologic or targeted therapy to start if a patient has not responded to methotrexate or other conventional DMARDs.
Should a patient who is about to start a biologic or targeted therapy choose a certain type over another? It’s a very common question, but these guidelines do not address it directly.
They do, however, say that if a patient has not responded to a biologic or targeted medication in a given class, switching to a biologic or targeted medication in a different class is conditionally recommended over taking a different drug in the same class. So, for example, if a patient has not responded to a TNF inhibitor, they should consider switching to a different type of therapy rather than a different TNF inhibitor.
Think carefully about whether or how to taper medications if a patient is considered to be in low disease activity or remission.
The 2015 guidelines recommended DMARD tapering for people who are in remission. The 2021 guidelines offer different tapering scenarios for patients in low disease activity or remission, noting that “careful tapering might be considered if the patient wishes to cut back on their use of DMARDs. However, patients should be closely evaluated during any taper, and if a flare occurs, the prior regimen should be reinstituted promptly.”
The guidelines note that stopping all DMARDs is associated with a moderate-to-high risk for flare and potential for irreversible long-term damage, so they recommend that patients stay on at least one DMARD if they choose to taper medication, rather than stopping all of them.
Essentially, the guidelines say that being on all DMARDs at their current dose is conditionally recommended over reducing the dose, reducing the dose is conditionally recommended over gradually stopping the medication, and gradually stopping medication is better than stopping abruptly.
Recommendations for Specific Comorbidities and Circumstances
The guidelines also offer specific treatment recommendations for patients who have certain co-occurring health conditions, including the following:
- Rheumatoid nodules
- Lung disease
- Heart failure
- Lymphoproliferative disorder
- Hepatitis B infection
- Nonalcoholic fatty liver disease
- Persistent hypogammaglobulinemia without infection
- Previous serious infection
- Nontuberculous mycobacterial (NTM) lung disease
If you have one of these conditions, you may want to speak to your provider about the guidelines to make sure your treatment plan is in line with the latest evidence.
In one example, the guidelines conditionally recommend methotrexate over other DMARDs for people with mild or stable lung disease. Although studies have indicated that pre-existing lung disease is a risk factor for methotrexate-related lung inflammation, more recent research has called this link into question and alternative DMARDs have also been linked to lung disease.
Interested in reading the full guidelines? You and your doctor can find them here.
Get Involved in Arthritis Research
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
Watch: Switching Rheumatoid Arthritis Medications
This video is part of an educational project from researchers at Yale University, Berkshire Medical Center, Carnegie Mellon University, Hospital for Special Surgery, CreakyJoints and the Global Healthy Living Foundation, and ArthritisPower. It was made possible with support from the Rheumatology Research Foundation. Watch more videos from this series here.
Dykes L. The 2021 Treatment Guidelines for Rheumatoid Arthritis. Rheumatology Network. June 9, 2021. https://www.rheumatologynetwork.com/view/the-2021-treatment-guidelines-for-rheumatoid-arthritis.
Fraenkel L, et al. 2021 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Care and Research. June 8, 2021. doi: https://www.doi.org/10.1002/acr.24596.
Interview with Liana Fraenkel, MD, MPH, adjunct professor of rheumatology at Yale School of Medicine and lead author of the new ACR guidelines
Interview with Shilpa Venkatachalam, PhD, MPH, Associate Director of Patient-Centered Research at the Global Healthy Living Foundation
Singh JA, et al. 2021 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis and Rheumatology. November 6, 2015. doi: https://www.doi.org/10.1002/art.39480.