Shilpa Venkatachalam, PhD, has the unique perspective of living with inflammatory arthritis as both a patient and Director of Patient-Centered Research Operations and Ethical Oversight at the Global Healthy Living Foundation (GHLF). Even after the workday ends, Shilpa continues to grapple with how to best treat rheumatoid arthritis, psoriatic arthritis, and other types of inflammatory arthritis.
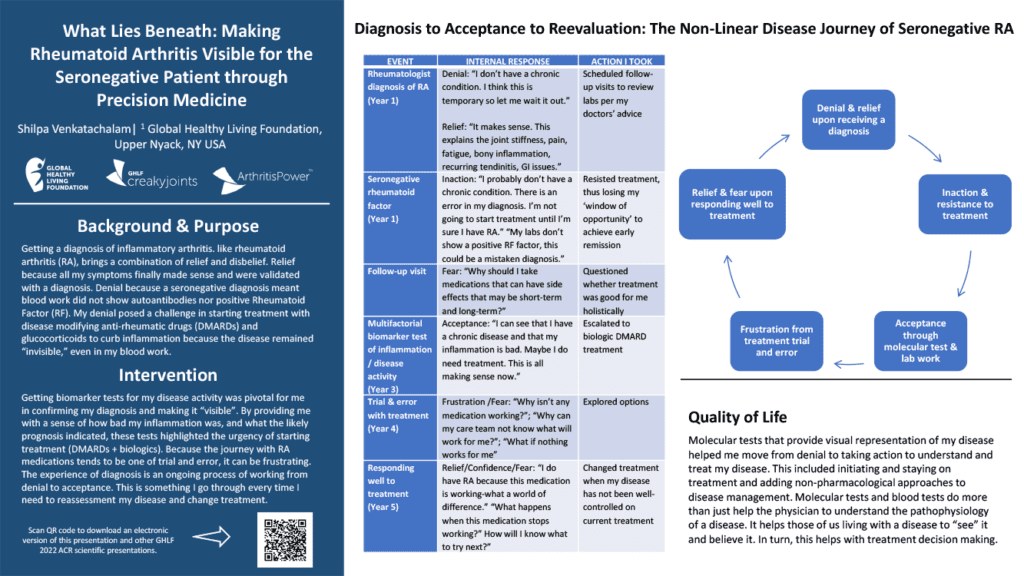
In a recent patient poster presented at the American College of Rheumatology Convergence (ACR) 2022, Shilpa shares what she’s learned from her non-linear journey of seronegative rheumatoid arthritis.
As a researcher and patient, Shilpa endeavors to bring the patient’s perspective into the work she does. She also wants to bring this perspective to the rheumatologists and clinicians at ACR so they may better understand the patient’s perspective at every stage of the disease, she explains.
“Only the patient can provide the patients’ perspective on living with seronegative RA,” says Shilpa. “If we want to understand the lived experience — the fatigue and diminished quality of life many patients struggle with every day — we need to hear from the patients. Patient-reported data can come only through the patient.”
Dealing with Denial
When someone is diagnosed with a potentially lifelong chronic illness, it is common to go through stages of grief. A diagnosis can bring relief in getting answers, yet it can be difficult to accept. Receiving a diagnosis of seronegative rheumatoid arthritis can magnify feelings of denial because, unlike seropositive rheumatoid arthritis, seronegative RA does not show a positive rheumatoid factor (RF) in bloodwork.
When Shilpa was initially diagnosed, she convinced herself that she did not have a chronic condition. “I think this is temporary so let me wait it out,” writes Shilpa in her poster. Despite the symptoms she had, such as fatigue, joint pain and stiffness, recurring tendonitis, and inflammation, Shilpa delayed treatment. She also feared potential side effects of medications and questioned whether the treatment was good for her holistically.
From Denial to Acceptance
Three years after her initial diagnosis, Shilpa decided to get a multifactorial biomarker blood test, which showed inflammation and disease activity. The results helped her begin to accept her diagnosis and start treatment on a biologic Disease-Modifying Antirheumatic Drug (DMARD).
“Molecular tests and blood tests do more than just help the physician to understand the pathophysiology of a disease,” says Shilpa. “It helps those of us living with a disease to ‘see it and believe it.’ In turn, this helps with treatment decision making.”
Finding Treatment
After five years of dealing with the frustrating process of trial and error to find the right treatment, Shilpa finally found a medication that worked for her.
Yet, like many people living with chronic illness, Shilpa remained worried that her medication would stop working: “How can my care team know what will work for me? What if nothing works for me?”
Now, seven years later, she wishes she took a more aggressive approach to treatment early on and wants to prevent others from making the same mistake. “Even if they do not see outward signs of disease progression, chronic inflammation is still at work,” says Shilpa, who urges patients to research and understand their diagnosis.
There are people working for us, looking for new medications, so we aren’t left without options,” she says. “You can live a good quality life if you take targeted medications regularly, combined with a healthy lifestyle — eat well, sleep well, keep moving — and build a support system. Ask for support.”
Shilpa finds it helpful to relate to the patient community within CreakyJoints and to keep communication lines open between herself and her doctor.
Messages of Hope
Here, she shares three lessons learned during her treatment journey — and hopes other patients take them to heart as they figure out what works to better manage their inflammatory arthritis.
- Don’t wait to get treatment. By resisting treatment, Shilpa says she lost her “window of opportunity” to achieve early remission. Joint damage is happening even if you don’t “see” it, and targeted medications are designed to slow the progression.
- It may take time to find the right medication for you. Shilpa acknowledges that it can take months for some people to find effective treatment. She suggests that those who are newly diagnosed speak to other patients who have been through a similar experience. “There’s a high and low feeling of finding a targeted medication that works for a while, but then needing to find a new medication when something stops working,” says Shilpa. “It’s important to know you’re not alone.”
- There is ongoing research to treat inflammatory arthritis, an autoimmune condition that affects people whether they are seropositive or seronegative. “There’s a whole team of researchers, physicians, and other clinicians, working to develop better, more targeted, medications with fewer side effects,” Shilpa reassures patients. “Keep that in mind and don’t give up hope.”
Be Part of Research with ArthritisPower
Join CreakyJoints’ patient-centered research registry and participate in voluntary studies about managing arthritis. Learn more and sign up here.
Interview with Shilpa Venkatachalam, PhD, MPH, Director of Patient-Centered Research Operations and Ethical Oversight at the Global Healthy Living Foundation.
Venkatachalam S. What Lies Beneath: Making Rheumatoid Arthritis Visible for the Seronegative Patient Through Blood Work. Arthritis & Rheumatology. November 2022. https://acrabstracts.org/abstract/what-lies-beneath-making-rheumatoid-arthritis-visible-for-the-seronegative-patient-through-blood-work/.