“You look really bloated.”
I don’t need to dig up a scientific study from Harvard to prove that telling someone they look fat is offensive (at best) and hurtful (at worst). And yet, that’s exactly what my friend recently said after meeting me for dinner an hour after I’d had an infusion for my rheumatoid arthritis.
She probably wasn’t wrong. After all, I’d just had a giant bag of liquid intravenously injected into my body to treat my rheumatoid arthritis. And it’s true that I’d mysteriously gained eight pounds since I started infusing and had been changing my anti-inflammatory NSAIDs like underwear, desperately trying to find one that didn’t make me retain water and feel like I was going to explode out of my skin.
So, yes, it’s definitely possible I looked like a pumpkin head at dinner. But that’s not the point. Who says that? Unfortunately, a lot of people say a lot of very inappropriate things to us folks with RA. Though many may have good intentions under the guise of worrying, they often don’t understand what it’s like to live with rheumatoid arthritis and why their words sting.
I talked with a group of people with rheumatoid arthritis for their take on the things it’s best to avoid saying — because we’ve heard them a gazillion times; because they’re offensive, judgmental, or dismissive; or just … because.
Share them with your friends, family, and even your doctors, so in the future they know what’s OK — and so not OK — to say.
1. Don’t say: “You’re too young to have rheumatoid arthritis!”
Rheumatoid arthritis (or psoriatic arthritis, or ankylosing spondylitis) is not that nagging pain your grandma complains about in her hip. RA is a very serious autoimmune disease, in which your immune system mistakenly attacks your own body’s tissues and causes severe joint pain, stiffness, severe fatigue, and sometimes deformity, usually in the hands, shoulders, knees, and/or feet. It affects men, women, and children of all ages.
RA is often confused for osteoarthritis, in which the protective cartilage on the ends of the bones wears down over time. OA affects millions of adults, and tends to occur with age. “I wish RA did not have the word arthritis in it,” says Mina Hartwell, 48, who was diagnosed with rheumatoid arthritis six years ago. “It’s awful that, because of that word, it is equated with an older person’s degenerative disease. There is a huge difference.”
Julie Anders, 55, has lived with RA for 12 years and is more forgiving when people say this to her. “I know it’s just coming from someone who really doesn’t know the difference or the fact that children suffer from it also,” she says. “It’s a complex disease so I don’t expect the general public to know that. I use it as an opportunity to share how RA can come on at any age and that it is an autoimmune disease.”
2. Don’t say: “At least you don’t have cancer. That would be worse. I mean, like, you won’t die from it.”
It’s not fair to compare RA to cancer because it’s apples to oranges. RA can be excruciating and is possibly life-threatening. Lea Dooley, 48, who was diagnosed with RA four years ago and fibromyalgia just last year, feels “fortunate to have been diagnosed during the golden age” of RA — during the recent emergence of biologic drugs that can help prevent long-term joint damage — but the truth is, if RA is left untreated, major organs can shut down. And research shows having RA does increase your risk of co-occuring diseases, such as heart disease, respiratory issues, and other problems that result from being under an assault of chronic inflammation.
3. Don’t say: “But you don’t look sick!”
There’s a reason #butyoudontlooksick is one of the more popular Instagram hashtags among the chronic illness community. While there is no cure for RA, patients can experience glorious periods of remission with little pain. Unfortunately, without warning or reason, RA can flare up from time to time and it can be painstaking to simply get out of bed or tie your shoes.
“When I am having a good day,” Hartwell explains, “you know like wearing makeup and a shirt with buttons, someone may says to me, ‘Oh, you must be better!’ Nope. Not better. Just feeling a little less miserable today but thank you for noticing!”
Check out this Instagram account if you hear #butyoudontlooksick one too many times.
4. Don’t say: “You’re probably just stressed out. Stress kills.”
Research remains inconclusive as to what role stress plays in the onset of rheumatoid arthritis. Some studies confirm the link; others, like a recent Dutch study, found no correlation between psychological stress and early signs of joint pain. Rheumatoid arthritis is thought to be caused by a number of factors, such as genetics, infection, or environmental factors like smoking, but nobody knows for sure yet.
When it comes to RA flares, stress can be a factor among a host of other triggers, but it doesn’t operate in a vacuum. So when people tell Briana Redulla, 33, she needs to “relax” to help control her disease, it really bugs her, especially because she lives in Hawaii, one of the most chill places on earth! Let’s not blame the victim, shall we?
5. Don’t say: “I’ve read that turmeric can cure your rheumatoid arthritis.”
Bottom line: There is currently no cure for RA. Otherwise we’d all be mainlining the golden Asian spice like fiends. Many people with RA swear that turmeric has anti-inflammatory healing properties and that’s perfectly fine — it works for them. The problem arises when complete strangers start pushing it more aggressively than a drug dealer.
“Much of the advice I get is from people pushing this or that current fad, with plenty of anecdotal evidence to support the claims, but very little, if any, scientific evidence,” explains Kandice Seeber, 45, who was diagnosed with RA and fibromyalgia about five years ago. “Things like tart cherry juice, CBD oil, deep blue rub, joint supplements. I get frustrated when people offer unsolicited medical advice when they are not qualified to do that, they don’t know my medical history or me, and they only have their own experiences to talk about.”
6. Don’t say: “Go gluten free!” or “Stop eating sugar!”
This May, at the age of 15, Charlie Kaufmann was diagnosed with polyarticular juvenile idiopathic arthritis and hospitalized for six weeks. The unsolicited advice he received was immediate, in particular, about what not to eat. “I’m a teenager,” Charlie says. “So when people tell me to cut out gluten or red meat, I think, ‘I just want to eat pizza and burgers with my friends!’”
Many people in the arthritis community cut out gluten because they think it can help relieve their symptoms, but the relationship between RA and gluten is controversial. There seems to be a connection between people who have celiac disease — an autoimmune disorder in which your body cannot digest gluten — and other autoimmune diseases, but there isn’t good scientific proof that people with RA or other kinds of arthritis who don’t have celiac will necessarily benefit from avoiding gluten.
There is some evidence that too much sugar is bad for RA. For example, a 2014 study published in the American Journal of Clinical Nutrition found that women who drank one or more sugar-sweetened beverage a day had a 63 percent greater risk of developing RA than women who never or rarely consumed the stuff. A diet filled with excess sugar is also bad for weight management and is linked to an increased risk of heart disease and diabetes, which RA patients are more vulnerable to.
Indeed, Dooley has noticed that just eating a cookie at a conference “killed” her knees and made her foot drag. But sometimes she just wants that darn cookie. And we don’t want you to tell us how to change our diets, especially when the data on how food choices affects RA isn’t exactly conclusive.
7. Don’t say: “You shouldn’t take so many drugs!”
Using natural remedies to help manage chronic illness is certainly having a cultural moment right now (thanks to the popularity of sites like Goop and TV shows like Dr. Oz’s, alongside the rise of cold-pressed juice chains and Paleo-inspired food brands), but many RA patients don’t want to be pressured into going the holistic route.
“I love the drugs that facilitate my health, so it bugs me when people are skeptical of drugs,” notes Patricia Flynn, 52. Medical choices are personal, so mind your own beeswax! (Unless, of course, beeswax is found to cure RA.)
8. Don’t say: “This would go away if you’d just lose weight”
“People seem to think that because I am a large person, I brought RA on myself,” says Seeber. “While this might be true, it’s incredibly dismissive. Weight loss is certainly a good idea and would help solve a lot of my health issues. The thing is, doing so while one is in a great deal of pain on a daily basis is very difficult if not impossible. I’ve lost weight many times — usually in short bursts when my pain is better — but always gain it back when I am in pain and can’t move as much. So it’s kind of a catch-22. If I could lose weight, my RA would improve. If I could just get rid of some of this RA pain, I could exercise more and lose weight. When people point out weight loss as an easy solution to RA, they don’t have the whole picture.”
9. Don’t say: “You should try yoga!”
In addition to their vociferous diet opinions, the peanut gallery has too many opinions about how people with RA should get exercise. A very common misconception is that yoga would be good for all people with rheumatoid arthritis, because of the stretching. This may be true for some, but not others.
When Jennifer, 44, was diagnosed three years ago, “everyone was always telling me I should do yoga,” despite the fact that her wrists were tender and sore. “‘No, I shouldn’t. Putting all of my weight on my inflamed joints is not helpful,’” she’d reply. “They’d say, ‘You need to strengthen your wrists.’” To which she would respond, “No, I don’t. I have a disease that’s in my blood and attacks my joints. I don’t have weak joints!”
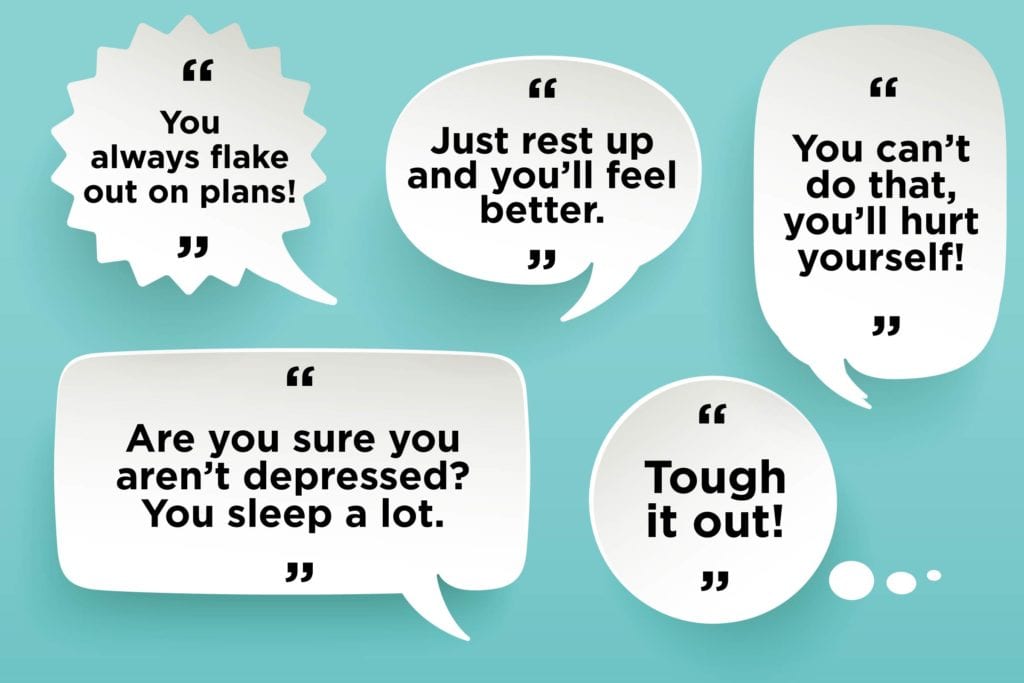
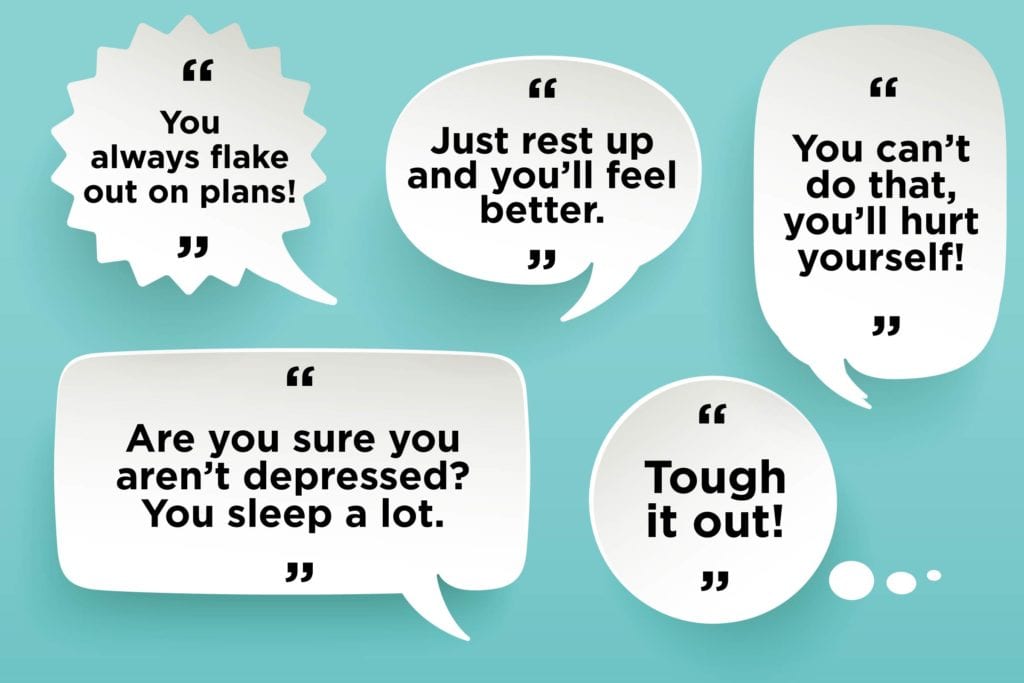
10. Don’t say: “Just rest up and you’ll feel better”
“Wrong!” insists Stefanie Foster Freeman, a holistic health coach and author of Life’s a Journey, Are You Packed? Living and Thriving with Juvenile Rheumatoid Arthritis. “You definitely don’t want to stiffen up. Moving actually helps my joints to feel better.” Every patient has different limits when it comes to exercise, but the research is pretty clear that for most people with RA, it’s important to move as much as possible to maintain flexibility, get good sleep, and keep that heart healthy.
My doctor told me I’d never run a marathon, and he’s right, I’m not going to run a marathon. (I never wanted to anyway!)
Though my friend called me bloated at dinner, she didn’t know that I work out four to five times per week and do intense HIIT training. I can’t run or jump but I modify the circuits and do as much as I can. Other RA patients find Pilates, walking, swimming, tai chi, weight lifting, or even cross country skiing, to be easiest on the joints. How RA patients choose to exercise is between them and their doctor.
11. Don’t say: “You can’t do that, you’ll hurt yourself!”
After Charlie’s hospital stay, his parents didn’t allow him to help out around the house anymore, doing chores like mowing the lawn; his coaches didn’t want him to play hockey. That upset him. “I don’t like when people say I can’t do the things I used to be able to do or put limits on me,” says Charlie. “They think everything hurts.” Like many people with RA, he has good days and bad days, where something new hurts and he can’t walk well or open doors. Nevertheless, he persists. “I’m playing hockey. I fix things around the house. I still want to help and I can depending on the day.”
12. Don’t say: “Are you sure you aren’t depressed? You sleep a lot.”
Lea Dooley’s husband Ted has always been supportive, but as a clinical psychologist, he worried about the number of naps she was taking, and it caused some issues between them. Chronic fatigue is a real issue for patients with rheumatoid arthritis, but research also backs up Ted’s concerns. One 2014 study found that nearly three-quarters of RA patients had some degree of depression; their symptoms correlated with the severity of their RA disease.
But mental health is a sensitive subject. It’s important to express concern about how a loved one is doing emotionally, but make sure you choose your words and tone carefully. You want to sound like you’re coming from a place of love and concern, not judgment.
13. Don’t say: “You always flake out on plans!”
One of the worst things about RA is its unpredictability. “You never know if it’s going to be a good day or a bad day,” says Eric Kops, 48, who’s one of the “super rare/unlucky” people who has both rheumatoid and psoriatic arthritis. “You can try to eat well and take care of yourself but there are no guarantees.” People without RA don’t understand that when you have a flare, you need to stay in, rest, and recover. “Even going to a movie can be too much when you are just sitting there and some parts of your body are just throbbing in constant pain.”
14. Don’t say: “Tough it out”
Kops has heard “push through it” more times than wants to, and it’s not just because he’s a guy. Redulla has also been lectured with “mind over matter” by well-meaning but ill-informed people. The power of positive thinking is lovely but let’s not overstate its ability to help people with RA feel less pain. Rheumatoid arthritis is a lifelong disease that is currently incurable. Friends and family, the best way to be an ally to someone with rheumatoid arthritis is to practice kindness, understanding, and patience. And, please, take a moment to think before you speak!
15. Do say: “Wanna read this?”
Instead of insisting that something — whether a so-called superfood, a new lifestyle tweak, or a breakthrough medication — will treat someone’s RA, you’re better off asking they’re interested in learning more. You can say, “Hey, I read a cool article about something related to RA. Can I send it to you?” Give us the option to look into it if and when we want to.
16. Do say: “Do you feel up to doing _____?”
“Ask me if I want to do something instead of assuming that I can’t,” Charlie explains. “Let me decide for myself what I can do. When people are overprotective, I know it’s coming from a good place of caring and love, but they don’t realize how upsetting it is. Even though I’m young, I need to make decisions for myself about my own health and body. I need to test myself and it’s going to change day by day.”
17. Do say: “I can see you’re struggling today. What can I do to help?”
This is a simple way of expressing sympathy for what someone else is going through, as well as compassion, by letting them know you want to help if they need it.
Watch: Talking to Your Family and Friends About Rheumatoid Arthritis
This video is part of an educational project from researchers at Yale University, Berkshire Medical Center, Carnegie Mellon University, Hospital for Special Surgery, CreakyJoints and the Global Healthy Living Foundation, and ArthritisPower. It was made possible with support from the Rheumatology Research Foundation. Watch more videos from this series here.
Subscribe to CreakyJoints
Get the latest arthritis news in your inbox. Sign up for CreakyJoints and hear about the latest research updates and medical news that could affect you.





