I have a problem with pain scales.
I don’t have anything against them as such. They work well for tracking acute pain from a single source, such as a wound. But as someone who lives with multiple kinds of chronic pain, I have no idea how to use them to record different kinds of pain from different sources at different times and intensities.
For example, how would I record this using a 0-10 pain scale? “Well, my rheumatoid arthritis used to give me lots of hand pain and foot pain but that’s well controlled at the moment. I also have ankylosing spondylitis (AS) and yesterday both of my sacroiliac joints were throbbing and achy for hours and this morning the muscles from my right glutes down through my thighs were super tight and extremely painful when I got out of bed and then they eased a little. Then I got this really sharp pain in the middle of my spine when I turned. Oh, and I had pins and needles down both legs from sciatica caused by my spondylolisthesis when I stood for a few minutes but that went away when I sat for a while.”
Impossible, right?
Pain Body Diagrams Are Problematic Too
I do better with the types of pain diagrams where you’ve got an outline of a body and you circle the areas that hurt. If I’m just marking which parts hurt at that exact moment, that’s easy. If I’ve got multiple parts hurting for different reasons, I’ve been known to color code my charts. (Over the top, I know. But you do what you gotta do.)
If I have to use an outline diagram to show where I’ve felt pain over the last week, that’s a different story. It just ends up looking like something a toddler would produce after some free reign with crayons.
I believe that charts like these have an important role in helping clinicians and researchers measure disease activity and progression over time but they rely heavily on the patient’s interpretation of pain and they need to be considered alongside the patient’s reports of functionality and circumstances.
Case Study: My Mechanical and Inflammatory Back Pain
Here’s another example.
Last month, I had a cortisone injection into my right sacroiliac joint. I’ve got a range of different back issues — some are mechanical and some are inflammatory.
The mechanical issues include periodic muscle aches from an area of scar tissue over the back of my right rib cage from lung surgery years ago. Like many people, I also get neck and shoulder pain from tight muscles if I’ve been stressed or hunched over a computer for too long.
I’ve also got a condition called spondylolisthesis, which is when one vertebrae has slipped forward over the one beneath it, causing some pinching of the surrounding nerves. This is related to a 20-millimeter difference in my hip height that gradually developed over several decades.
Then there is the pain caused by varying levels of inflammation in my sacroiliac joints, especially the right one (that’s where the AS comes in). As for the sudden sharp twinges in the middle of my spine, they are yet to be diagnosed, but could be my AS progressing or osteoarthritis.
One or more of these issues had been causing me lots of pain across my lower back and especially on the right side, turning just before the hip and shooting down the muscles of my thigh and sometimes my calf. This was getting very bad in the mornings, so I went to see my trusted musculoskeletal physician.
We decided to focus on that area of pain as the priority to treat and agreed that a cortisone injection would be my best bet. The trouble was it was hard to know exactly which spot was the main source of pain. Was it the pinched nerve roots in the spine or the inflammation in the right SI joint?
We decided that the SI joint was the most likely culprit so that’s where I had the injection the following week.
Tracking My Results with a Pain Chart
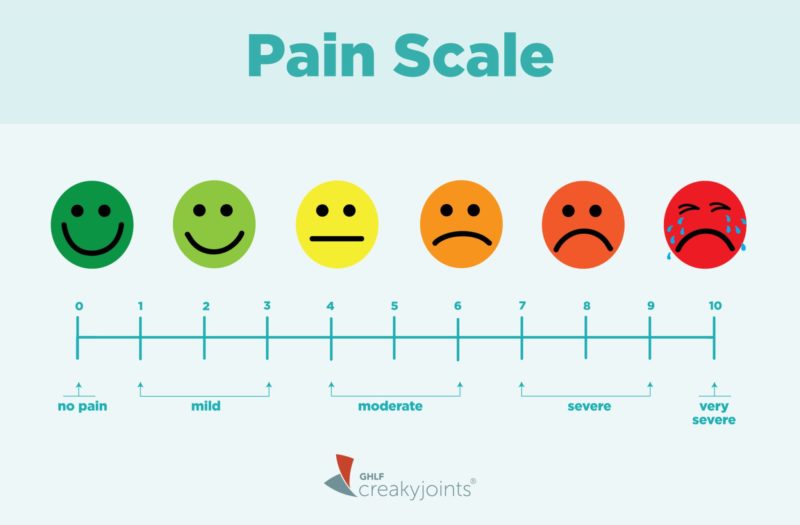
On the day of my injection, I was asked to use the 0 to 10 pain scale before the procedure. I tried to focus on just that area and randomly picked 5. It wasn’t the worst pain I’d ever experienced, but I was limping a fair bit. I could just have easily said 4 or 6. After the injection, I was given a pain chart to complete at regular intervals that day and then daily until day 12.
Wonder of wonders: Although the injection itself was uncomfortable, for the rest of that day and all the next day, my pain levels throughout my body were at a big, fat zero. Yay! I hadn’t felt that good in ages.
Then came day 3. I started getting pain around my SI joints and a bit in my right thigh muscles. I rated my pain for that day at 6 and needed extra pain meds and an anti-inflammatory (on top of my daily doses and other meds that I had continued all along).
For the remaining days, my SI joint pain varied between 4 and 6, despite extra meds and extra stretches to try to relieve the pain. I also had several strong twinges around the middle of my spine and periods of pins and needles down both legs from sciatica.
But all my pain chart showed was the numbers I’d picked and my super brief comments about the extra meds I took each day. I also squeezed in a note saying that the pain was mostly from my SI joints and that I was unsure if the procedure had helped or not.
My Forgotten Pain
I sent that chart back to my doctor and discussed it during my follow-up appointment. We were both disappointed that the full pain relief hadn’t lasted and we weren’t quite sure about the outcome. We decided to give it a bit more time and to see what my rheumatologist says when I see him soon. I may have an MRI to investigate further.
But the day after that follow-up appointment, I had a lightbulb moment.
I had been so focused on tracking the SI joint pain that I had failed to notice the muscle pain in my right glutes and thigh muscles had almost gone away. How could I not have noticed that? It was the reason I wanted the injection in the first place.
I emailed that extra bit of information to my doctor that day and we both agreed that the injection had made some difference after all.
And that is why I have a problem with pain scales. If I had been tracking *all* my pain spots in a holistic way over that period I’m sure I would have noticed the absence of that particular pain pretty quickly. As it was, I was just focusing on one area — so I lost sight of the big picture.
I much prefer my personal pain and medication diary. I use it to jot down a few lines about any changes in drug doses, pain spots, pain levels, and my general functionality. Again, this might seem over the top, but it’s become one of my coping tools for managing multiple conditions.
Now, how would I rate the effectiveness of pain scales on a pain scale? Hmmm… I’ve got no idea.
Track Your Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Learn more and sign up here.