Odds are you’ve heard of a biopsy, or maybe you’ve had one yourself. It’s a procedure during which a small amount of cells or tissue is removed from your body for examination. Biopsies can help diagnose cancer, liver disease, polycystic ovarian syndrome, and many more conditions.
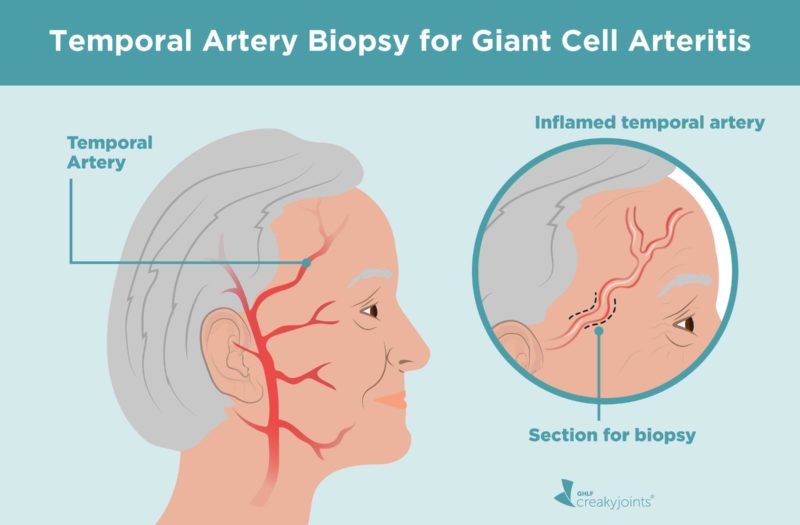
One type of biopsy, called a temporal artery biopsy, involves taking a piece of blood vessel from the side of your head. It’s the best way to identify a potentially serious disease called giant cell arteritis (GCA), also called temporal arteritis. Accurate diagnosis and early treatment of GCA can help prevent such complications as blindness, aneurysms, and stroke.
Here’s what you should know about getting a temporal artery biopsy to figure out if you have GCA.
Giant Cell Arthritis Causes, Symptoms, and Importance of Diagnosis
“GCA is a type of vasculitis, an inflammatory condition involving the arteries,” says Sara Tedeschi, MD, a rheumatologist at Brigham and Women’s Hospital in Boston, Massachusetts. When you have GCA, your blood vessels narrow, which can slow blood flow. “[It] affects large arteries such as the aorta — the major artery that carries blood from the heart to the rest of the body — and its branches, including the temporal arteries in the head,” she explains.
GCA is thought to be an autoimmune disease, which occurs when your immune system malfunctions and begins attacking healthy tissue. Doctors aren’t exactly sure what causes GCA, but genetics and environmental factors likely contribute.
Age, sex, and race are risk factors for developing the disease. “GCA occurs exclusively in adults, usually at least 50 years old but often older,” Dr. Tedeschi explains. Women are twice as likely as men to develop GCA, and the condition is much more common among Caucasians than people of other races. About half of people with GCA also have a condition called polymyalgia rheumatica, says Dr. Tedeschi, “which causes pain and stiffness in the shoulders and/or hips, usually on both sides of the body.”
Early GCA signs include fever, fatigue, and loss of appetite, and often look like the flu. Additional commonly reported symptoms are:
- Sudden, severe headaches, usually around the temples
- Persistent pain or tenderness of the scalp, or in the area around the temples
- Vision problems, including double vision, blurred vision, or vision loss
- Jaw pain or cramps, especially when chewing or speaking
Other symptoms may include (but are not limited to) dizziness and coordination problems, tongue pain, constant sore throat, and unintended weight loss.
Pinpointing a GCA diagnosis can be tough, since symptoms resemble those of many other illnesses. For example, the characteristic head pain may be confused with headache disorders. Jaw and facial discomfort can lead to a misdiagnosis of temporomandibular joint (TMJ) arthritis (arthritis of the jaw). Since the illness occurs in older people, vision problems may be attributed to aging. And that’s not all: Other types of vasculitis, infections, some cancers, and severe atherosclerosis (a hardening of the blood vessels) are just a few of the illnesses that GCA can mimic as well.
Since the complications of GCA be quite serious if the disease is left untreated, thorough testing and accurate diagnosis is critical. “The most feared complication of GCA is blindness, since GCA can cause inflammation of the arteries that supply the retina in the eye,” says Dr. Tedeschi. Once your vision is gone, it doesn’t typically come back. GCA is also linked to a higher lifetime risk of aneurysms, or bulges in weakened artery walls. Aortic aneurysm, which affects the artery that brings blood away from the heart, can be deadly. Stroke is another life-threatening complication of GCA, though it is relatively uncommon.
How GCA Is Diagnosed
There’s no one test to confirm GCA. To help reach a diagnosis, your doctor will note your symptoms and take your medical history. They’ll also conduct a physical exam, partly focusing on the arteries in your temples. If you have GCA, the arteries may feel hard or tender.
Then you’ll require some testing. “Typically, if a doctor suspects GCA, the first tests ordered are blood tests looking for inflammation,” says Dr. Tedeschi. These include the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) blood tests; high levels of either signify inflammation suggesting GCA.
Imaging may help pinpoint GCA, as well. “A specialized ultrasound … can be performed in some medical centers to evaluate for inflammation of the temporal arteries and the large arteries in the upper chest,” explains Dr. Tedeschi. Other types of imaging studies may be performed, “if the doctor suspects inflammation in the aorta [in the chest] or its branches in the chest and upper extremities,” she adds.
While blood tests and imaging are helpful, there’s one test often prized above all others.
“The gold-standard test for GCA has traditionally been a temporal artery biopsy showing active inflammation of the temporal artery,” she says. “If your doctor recommends that you have a temporal artery biopsy, this generally means they have a high level of suspicion for GCA.”
What Happens During a Temporal Artery Biopsy
“A temporal artery biopsy is an outpatient procedure that is typically performed by a vascular surgeon or ophthalmologic surgeon,” says Dr. Tedeschi. You won’t be put under general anesthesia or have to stay overnight in a hospital. Your provider will let you know about any special preparations beforehand.
To begin, the surgeon will mark the skin around your temples where they’ll make an incision. Then, they’ll use local anesthesia to numb the area. A small piece of your temporal artery will be removed and sent to a pathology lab. Finally, your incision will be stitched up or closed with staples.
As a temporal artery biopsy is an outpatient procedure, you can go home once it’s finished. Over-the-counter pain relievers should be enough to treat any discomfort. You’ll likely be given antibiotic ointment for the incision area, which you should keep dry for a few days after the procedure. Results often arrive back within a week.
Complications following a temporal artery biopsy are uncommon, and the test is not seen as dangerous. “This is generally considered a low-risk procedure,” says Dr. Tedeschi. Rarely, patients experience bleeding, scarring, wound separation or infection, or facial nerve damage.
How a Temporal Artery Biopsy Is Used to Diagnose GCA
To confirm a GCA diagnosis, a pathologist will review your biopsy, “to look for disruption of the normal structure of the temporal artery and for the presence of inflammatory cells within the walls of the artery,” Dr. Tedeschi says. In people with GCA, some of these cells, called giant cells, will be unusually large — hence the name.
Though “incredibly useful,” temporal artery biopsies aren’t perfect. “Unfortunately, a temporal artery biopsy can sometimes be negative [normal] in a patient with GCA because GCA can ‘skip’ areas in the artery, leaving some areas unaffected,” says Dr. Tedeschi. If doctors are uncertain about your results, you may have to get a second temporal biopsy — this time, around your other temple.
After a GCA Diagnosis: GCA Treatment
Treating giant cell arteritis early is key to preventing complications and usually leads to good health outcomes. Your doctor will typically use corticosteroid drugs, which ease symptoms quickly and lower the chance of vision loss. Patients often start to feel better after a few days but must continue taking the medication for years to keep inflammation in check. Sometimes low-dose methotrexate — given as tablets or injections — is added alongside steroid treatment for GCA.
Seeing your doctor regularly is vital during this time, since long-term corticosteroid use can come with serious side effects, such as osteoporosis and increased infection risk.
To note: Quick treatment is vital to avoiding blindness, so you may be started on corticosteroids before your doctor verifies you have GCA with testing. To confirm a diagnosis, a temporal artery biopsy can be performed up to two weeks after treatment begins.
Corticosteroids may not be your only option. In 2017, the U.S. Food and Drug Administration approved the biologic medication tocilizumab (Actemra) for GCA treatment. The medication is taken via a self-administered injection at home. Speak with your doctor about whether it might be right for you. Learn more about taking tocilizumab for GCA.
Whatever your treatment, it’s important to attend follow-up visits and make health care providers aware of your GCA diagnosis, since it can affect your risk for aneurysm and other complications even years later.
Keep Reading
Biopsy. MedlinePlus. https://medlineplus.gov/biopsy.html. Published November 5, 2019.
FDA approves first drug to specifically treat giant cell arteritis. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-drug-specifically-treat-giant-cell-arteritis.
Giant Cell Arteritis. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Giant-Cell-Arteritis.
Giant cell arteritis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/giant-cell-arteritis/symptoms-causes/syc-20372758. Published September 27, 2018.
Giant Cell Arteritis – Bone, Joint, and Muscle Disorders. Merck Manuals Consumer Version. https://www.merckmanuals.com/home/bone-joint-and-muscle-disorders/vasculitic-disorders/giant-cell-arteritis. Last full review/revision June 2019.
Giant Cell Arteritis (Temporal Arteritis). Rheumatology Advisor. https://www.rheumatologyadvisor.com/home/decision-support-in-medicine/rheumatology/giant-cell-arteritis-temporal-arteritis. Published January 20, 2019.
How biopsy procedures are used to diagnose cancer. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/cancer/in-depth/biopsy/art-20043922. Published July 9, 2019.
Interview with Sara Tedeschi, MD, Brigham and Women’s Hospital
Nys, Marguax, et al. A case of giant cell arteritis and polymyalgia rheumatica misdiagnosed as temporomandibular dysfunction. Oral Science International. July 2018. doi: https://doi.org/10.1016/S1348-8643(18)30006-5.
Polymyalgia Rheumatica. National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/polymyalgia-rheumatica. Published September 30, 2019.
Prednisone and other corticosteroids: Balance the risks and benefits. Mayo Clinic. https://www.mayoclinic.org/steroids/art-20045692. Published October 9, 2019.
Rana AQ, et al. Giant cell arteritis or tension-type headache?: A differential diagnostic dilemma. Journal of Neuosciences in Rural Practice. 2014. doi: 10.4103/0976-3147.140005.
Schmidt WA. Ultrasound in the diagnosis and management of giant cell arteritis. Rheumatology. 2018. doi: 10.1093/rheumatology/kex461.
Stone J, et al. Long-Term Outcome of Tocilizumab for Patients with Giant Cell Arteritis: Results from Part 2 of a Randomized Controlled Phase 3 Trial [abstract]. Arthritis & Rheumatology. 2019. https://acrabstracts.org/abstract/long-term-outcome-of-tocilizumab-for-patients-with-giant-cell-arteritis-results-from-part-2-of-a-randomized-controlled-phase-3-trial.
Temporal Arteritis. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/15674-temporal-arteritis.
Temporal Arteritis | Giant Cell Arteritis. MedlinePlus. https://medlineplus.gov/giantcellarteritis.html. Published November 12, 2019.
Temporal Arteritis aka Giant Cell Arteritis and Temporal Artery Biopsy Technique. University of Iowa Health Care. https://medicine.uiowa.edu/iowaprotocols/temporal-arteritis-aka-giant-cell-arteritis-and-temporal-artery-biopsy-technique.
Temporal Artery Biopsy. EyeWiki. https://eyewiki.aao.org/Temporal_Artery_Biopsy. Published October 21, 2019.
Temporal artery biopsy technique. UpToDate. https://www.uptodate.com/contents/temporal-artery-biopsy-technique.
What Is Giant Cell Arteritis? American Academy of Ophthalmology. https://www.aao.org/eye-health/diseases/what-is-giant-cell-arteritis. Published September 11, 2019.
Wiszniewska M, et al. Giant Cell Arteritis as a Cause of First-Ever Stroke. Cerebrovascular Diseases. 2007. doi: 10.1159/000104482.
Wolinsky H. Can Imaging Replace Biopsy for GCA Diagnosis? MedPage Today. https://www.medpagetoday.com/meetingcoverage/acr/75840. Published October 22, 2018.