If you feel tired all the time and have muscle aches and pains, you might think you’re coming down with the flu or another illness. But if your symptoms have been persisting for weeks or months and you also have insomnia, GI distress, or cognitive issues like “brain fog,” consider making an appointment with your general practitioner to discuss the possibility of having fibromyalgia.
Here are other common fibromyalgia symptoms to be aware of.
What Is Fibromyalgia?
Fibromyalgia is a disorder that causes widespread chronic pain and tenderness. According to the American College of Rheumatology, fibro (as many patients call it) is more common in women than in men and also common among people with arthritis or chronic pain, such as rheumatoid arthritis, ankylosing spondylitis, or lupus. Fibromyalgia can occur at any age but most often first strikes in middle age.
Doctors don’t know exactly what causes fibromyalgia, but they know that the condition is not due to an autoimmune disease, systemic inflammation, or physical joint or muscle disorder.
“People who have fibromyalgia have a reduced pain threshold,” says Frederick Wolfe, MD, a rheumatologist and fibromyalgia expert in Wichita, Kansas, who helped create the original and updated fibromyalgia diagnostic criteria from the American College of Rheumatology. “If you stick your finger in someone’s chest who has fibromyalgia, when you press down, they will say that it hurts. The pressure is more painful than in someone who doesn’t have fibromyalgia.”
Diagnosing Fibromyalgia Can Be Difficult
There’s no single test (such as a blood test or an imaging test like an X-ray) that can confirm a diagnosis of fibromyalgia. Rather, fibromyalgia is considered a “diagnosis of exclusion,” which means that doctors first have to rule out other health problems.
Make an appointment with your family doctor or rheumatologist (if you already have one) to discuss your symptoms. It could be helpful to download a fibromyalgia pain log to track your symptoms, the severity of pain, and how your lifestyle is impacted and bring that to the physician’s office.
You can also use our ArthritisPower app to track your symptoms and share your results with your doctor.
Diagnosing fibromyalgia is often challenging, says John Dombrowski, MD, anesthesiologist and pain management specialist at The Washington Pain Center, Washington, D.C. “It can be a challenge for the physician but also for patients,” he says. “When you have a headache or a broken bone, you can point to the problem. With fibromyalgia, the symptoms can be somewhat vague.”
Here’s why fibromyalgia tends to be tricky to diagnose:
1. You might not be visiting the correct doctor
While your first course of action will probably be to talk to your primary care doctor, you may want to ask for a referral to a rheumatologist. “The people who mainly work with fibromyalgia are rheumatologists because fibromyalgia is a rheumatologic problem,” says Dr. Dombrowski. A visit to a rheumatologist may involve tests to rule out health problems that can have similar symptoms as fibromyalgia, including Lyme disease, rheumatoid arthritis (RA), axial spondyloarthritis, and osteoarthritis.
It’s wise to get a specialist involved who’s used to dealing with fibromyalgia patients for diagnosis and initial treatment. Once you have a fibro diagnosis, a pain management specialist like Dr. Dombrowski can offer customized treatments to fibromyalgia patients for whom chronic pain is an issue.
If you can’t get to a pain specialist or rheumatologist because there isn’t one available in your area right away, talk to your primary care doctor about your symptoms and mention that you think it could be fibromyalgia. They could try to diagnose it themselves and treat the symptoms to see if that helps.
2. Your doctor might not be screening you properly
One of the reasons that fibromyalgia can be difficult to diagnose is that doctors spend time and resources searching for diseases that could be causing all of the various symptoms of fibromyalgia, says Dr. Wolfe. If your doctor doesn’t suspect fibromyalgia — and depending on the exact nature of your symptoms and related diseases, they might not — they might land on a different condition, such as depression or irritable bowel syndrome. Seeing a rheumatologist or doctor who is experienced in treating fibromyalgia patients may accelerate your time to getting diagnosed.
3. Fibro pain is often invisible
It’s important to verbalize exactly where on your body you experience pain, and to describe how the pain feels, what brings it on, how long it lasts, and what, if anything, makes it feel better. While someone with, say, RA can often point to a specific body part (like the hand) that has swelling, redness, and stiffness in addition to pain, someone with fibromyalgia tends to experience widespread pain and tenderness in larger areas, like specific quadrants of the body. Some people with fibromyalgia experience tingling or burning sensations, along with pain, in areas of the body, as well as significant fatigue.
4. Fibro can occur with other diseases
People can have fibro at the same time as other diseases, such as inflammatory arthritis or osteoarthritis. They’re all chronic pain conditions, but a rheumatologist should be able to ask questions and do lab or imaging tests that help distinguish them. A scenario is that a patient might have a diagnosis of RA and is taking medication that reduces inflammation but still experiences pain. In this case, the pain may be due to fibro (or something else) rather than from the RA. One study published in the journal Annals of Rheumatic Diseases found that 14 percent of the RA patients who participated in the research also fulfilled fibromyalgia criteria. If you have RA or OA and think you might also have fibromyalgia, bring it up to your rheumatologist to see if they can treat those symptoms of fatigue and overall pain as well.
Physical Exam and Medical History for Diagnosing Fibromyalgia
In order to diagnose fibromyalgia, your doctor should ask you about the following symptoms and their severity: pain you’ve felt throughout the past week, fatigue, cognitive problems, and whether you wake up feeling tired. They will likely want to know about specific pain, sensitivity, and tenderness that you feel in certain areas of the body.
In addition, your doctor should also ask about other symptoms, since fibromyalgia commonly coexists with other seemingly unrelated health issues, including irritable bowel syndrome (IBS), jaw pain from clenching, headaches, frequent urination, and anxiety or depression.
“An over-stimulated nervous system could lead to undiagnosed stomach issues, as well as jaw pain and headaches from clenching your jaw in response to the overall pain,” says Dr. Dombrowski. This is why it’s so important to have a physician who listens to your symptoms and can make the connection among them. “Eighty percent of the diagnosis is the physician listening.”
Older vs. Newer Criteria for Diagnosing Fibromyalgia
The criteria (or “rules”) for diagnosing fibromyalgia have changed over the last decade. Criteria from the American College of Rheumatology (ACR) first published in 1990 required:
- Presence of pain on both sides of the body
- Presence of pain above and below the waist
- Presence of at least 11 out of a possible 18 tender points
- Pain present for at least three months
- Pain not due to another disorder
However, more recent criteria have downplayed the role of the tender points in clinching a fibromyalgia diagnosis. The ACR’s updated fibromyalgia diagnostic criteria from 2010 — created with the help of Dr. Wolfe — suggests using questionnaires that assess pain and related symptoms, called the widespread pain index (WPI) and symptom severity scale (SSS).
The WPI asks where you felt pain in specific areas of the body, noting a “1” for each area. The SSS assesses how the pain feels in terms of fatigue, cognitive symptoms, and how you feel when you wake up, on a scale of 0 (no problems) to 3 (severe and continuous).
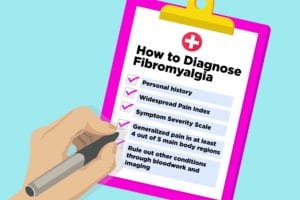
Today, doctors diagnose fibromyalgia based on the following general guidelines:
- Using the Widespread Pain Index and Symptom Severity Scale when (WPI) ≥7 and the Symptom Severity Scale (SSS) score ≥5, OR WPI 4–6 and SSS score ≥9.
- Generalized pain, defined as pain in at least four of five regions (left upper, right upper, left lower, right lower, low back) is present.
- Symptoms have been present and consistent for at least three months
- Counting tender points (not required)
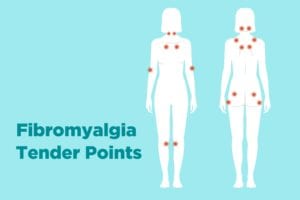
The Role of Counting Tender Points
When doctors would diagnose fibromyalgia years ago, they would count tender points and track those tallies over time to determine if the patient’s condition was getting better or worse. They would apply pressure to 18 (sometimes 19) specific points on the body where fibromyalgia patients tend to experience more pain and sensitivity. The tender points, which occur on both sides of the body, include:
- Lower neck in front
- Edge of upper breast
- Arm near the elbow
- Knee
- Base of the skull in the back of the head
- Hip bone
- Upper outer buttock
- Back of the neck
- Back of the shoulders
Now the tender point counting method is not recognized as a standardized measure for diagnosing fibromyalgia and determining whether the condition is getting better or worse. That’s because research found that tender points were only present in about 50 percent of fibromyalgia patients. Many people didn’t fulfill the pain criteria for these specific areas, but in general had “pain all over” or in specific areas. Counting and assessing tender points was seen as arbitrary and excluded people who had fibro but didn’t fulfill these criteria.
Counting and evaluating tender points is still being used today by some doctors but shouldn’t be used exclusively for a fibromyalgia diagnosis. You can have fibromyalgia without having pain in these specific tender points.
Tests for Diagnosing Fibromyalgia
There is no specific blood test to diagnose fibromyalgia. Your physician may take blood to screen for other diseases and rule other diseases, such as hypothyroidism (underactive thyroid gland), polymyalgia rheumatica, rheumatoid arthritis, or lupus.
Tests such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) detect inflammation in the body. They should be elevated in diseases like rheumatoid arthritis but not in fibromyalgia. (One study found that CRP levels were reported higher in those people who had been diagnosed with fibromyalgia, but high BMIs and other chronic diseases might explain that association.)
If your CRP tests come back with low or medium levels and ESR tests show low inflammation, that might eliminate other diseases and point your doctor in the direction of diagnosing fibromyalgia. Emerging research using vibrational spectroscopy (an advanced blood test) may help identify specific protein biomarkers in the blood that differentiates fibro from other disorders. But this test isn’t expected to be ready for mainstream use for another five years at least.
Imaging Tests for Diagnosing Fibromyalgia
While arthritis that has caused joint damage can be seen on an X-ray, fibromyalgia does not show up on X-rays. So if you have fibro symptoms like widespread body pain (or in those specific areas mentioned above) but X-rays don’t show joint damage, that could be another indicator that your symptoms are due to fibromyalgia.
In research studies, functional brain imaging tests in people with fibromyalgia have noted abnormal pain processing in specific areas of the brain. Magnetic resonance spectroscopy (a noninvasive test that measures biochemical changes in the brain) found higher concentrations of the neurotransmitter glutamate in specific pain-related areas in fibromyalgia patients. Researchers have used this technology during studies but it’s not yet being done in doctor’s offices to help diagnose patients. Your physician should be able to diagnose fibromyalgia using the methods outlined above.
How Doctors Know It’s Fibromyalgia and What Happens Next
Once your doctor has assessed whether you meet the criteria for fibromyalgia diagnosis and has ruled out other conditions, they may suggest prescription medication and lifestyle modifications to treat and manage fibromyalgia.
Your doctor may recommend certain antidepressant medication, which can not only treat depression, but also address pain and fatigue linked with fibromyalgia. Another category of commonly prescribed medication for fibro is anti-seizure drugs that can also help with the nerve-related pain from fibromyalgia. These include gabapentin (Neurontin) and pregabalin (Lyrica).
Lifestyle changes are a core part of fibro treatment. “I suggest patients eat a healthy diet and practice relaxation techniques, like meditation, stretching, yoga, and physical therapy,” says Dr. Dombrowski.
Therapies like cognitive behavioral therapy (CBT) and talk therapy may be recommended, as well as acupuncture, massage therapy, and chiropractic help to reduce pain and symptoms. Getting regular exercise — even in very small increments at first — is important. It’s key to get enough sleep and practice stress management and self-care to help with fatigue from fibro.
Once your rheumatologist or pain specialist has come up with a treatment plan, you can continue to see them or work with your primary care doctor to manage symptoms and adjust prescriptions and lifestyle habits as needed.
Support for Managing Fibromyalgia
Chances are, if you’re seeing a rheumatologist or other doctor because you have concerns about having fibromyalgia, you’ve already seen quite a few health care providers by now. We know this process can be exhausting and exasperating. We are here for you to help make things easier. Become part of the CreakyJoints community (you can sign up in the upper right corner of our site) and follow us on Facebook and Twitter for ongoing support and education.
Get a more specific list of fibromyalgia symptoms and check out these tips for living better with fibromyalgia from fellow patients. Stay up to date here on all of our fibromyalgia news and resources.