While no one knows what exactly causes fibromyalgia, doctors do know a few things about the condition: The widespread chronic pain disorder seems to involve the nervous system; affects 2 to 4 percent of Americans, mostly women; and commonly occurs in people who have other types of musculoskeletal pain, such as different kinds of arthritis.
But unlike many musculoskeletal conditions, fibromyalgia isn’t an inflammatory or autoimmune disease — when your immune system, which normally protects your body from infection, turns against itself and attacks your own cells and tissues. That can produce chronic inflammation that can eventually damage your body. Fibromyalgia is also not a joint or muscle disorder caused by physical injury.
Instead, experts think that fibromyalgia is neurological in nature.
“Fibromyalgia is a disorder in which the sensitivity to pain has been turned up in the brain,” says J. Michelle Kahlenberg, MD, PhD, an associate professor in the division of rheumatology at the University of Michigan Medical School in Ann Arbor. “Chemical transmitters in the brain have gotten reprogrammed so that they are firing pain signals with very minimal stimuli. A squeeze of the arm, a shake of the hand, a touch on the shoulder — all of those things can be very painful for people with fibromyalgia.”
Misdiagnosing Fibromyalgia: Why It’s Common
There’s no test that can diagnose fibromyalgia, so when fibromyalgia symptoms — which include widespread pain, sensitivity to touch, sleep issues and fatigue, brain fog, gastrointestinal distress (bloating and diarrhea), and mental health issues like depression and anxiety — propel you into the doctor’s office, your provider must first rule out other conditions that could be responsible for your fibro symptoms.
“That’s why fibromyalgia can be underdiagnosed, because we have to look for everything else first. On the other hand, fibromyalgia can also be overdiagnosed, because there’s no specific blood work or imaging tests that we can do to diagnose it,” Dr. Kahlenberg explains.
Studies bear this out. In a recent study published in the journal Arthritis Care & Research, researchers discovered that doctors at a university rheumatology clinic over-diagnosed fibromyalgia in 43 patients out of 121 who met the criteria, and missed it entirely in 60 patients.
Here’s why: To diagnose fibromyalgia, doctors rely on your description of symptoms, including pain and fatigue, and how long you’ve been having them. Sometimes they also use something called tender points criteria — where your provider presses 18 or 19 points along your body from your head to your knees as you rate the pain. And even though there’s no longer an exact number of tender points that determines whether you have fibromyalgia, some doctors may be reluctant to diagnose the condition if you have too few.
Another reason the disease is underdiagnosed: “There are a lot of patients who have fibromyalgia with another disorder,” says Chris Morris, MD, a rheumatologist with Arthritis Associates in Kingsport, Teneessee. “We immediately say, ‘Oh it’s that disease!’ without realizing or recognizing that some of their symptoms certainly put them in the category of fibromyalgia.”
This is a really important point. If you’ve been diagnosed with fibromyalgia (which can be notoriously challenging to manage with medication) and continue to experience pain and other symptoms despite treatment, it may be the case that you have another condition — say, rheumatoid arthritis (RA) or axial spondyloarthritis (AxSpA) — instead of or in addition to your fibro.
If you’ve been diagnosed with a different disease like rheumatoid arthritis but continue to experience pain despite taking medications to control inflammation, it could be that you also have fibromyalgia, which needs to be treated separately from your arthritis.
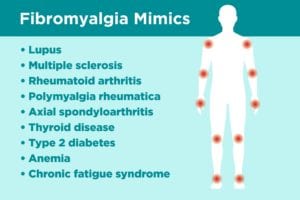
Here is a list of common health issues that can have similar symptoms as fibro. If you suspect you could have any of them, share your concerns with your doctor and ask if further testing is right for you.
1. Lupus
Like fibromyalgia, lupus affects women primarily, who experience pain in their joints as well as fatigue, memory issues, and headaches and stomachaches. But unlike fibro, lupus is an autoimmune disorder that causes widespread inflammation throughout the organs, especially the kidneys, lung tissue, heart, and brain.
Other physical symptoms of lupus can be very different too: “[Lupus can cause] skin rashes, hair falling out — not just a little bit of hair in the drain, but bald spots on the head,” notes Dr. Kahlenberg. There is also recurring pericarditis, which is chest pain brought about by inflammation of the tissue surrounding the heart, and kidney damage.
To rule out lupus, primary care providers usually order a blood test called an ANA test that measures certain autoantibodies in your body (a sign that your immune system is attacking normal cells instead of harmful bacteria or viruses). But a positive ANA doesn’t necessarily mean you have lupus. “A lot of people have a positive ANA for many reasons, most of which have to do with being exposed to some virus that had a little bit of overlap with their body’s tissues,” says Dr. Kahlenberg.
Of course, patients with lupus can also have fibromyalgia, which is why Dr. Kahlenberg also gives them the Michigan Body Map test, which allows patients to pinpoint the locations on their bodies where they feel pain. “If patients score high enough on a widespread pain index, then that would be diagnostic of fibromyalgia,” she says.
But whether you have fibro along with lupus or just lupus alone, it’s important to get the right treatment so the lupus doesn’t progress and cause more organ damage, which can be life-threatening. So you’ll want to talk to your provider about a combination of medications (usually steroids and anti-malarial drugs) that can suppress your immune system.
2. Multiple Sclerosis
MS is another autoimmune disorder; it affects the brain and spinal cord and can damage the nerves involved. Some people with MS can lose their ability to walk or see, others can go into remission for long periods of time. On the surface, some of the symptoms of MS and those of fibromyalgia are similar: brain fog, fatigue, insomnia, and pain.
Other symptoms of MS are very different from those that occur in fibro, including blurred vision, unsteady gait, lack of balance, tremors, and slurred speech. Multiple sclerosis patients can have lesions on the brain, so doctors frequently order MRIs to rule out MS or another neurological disorder. A spinal tap — a sampling of spinal fluid that’s sent to the lab — can sometimes show antibodies associated with MS.
There’s no cure for MS, but there are injections and oral medications to slow its progress as well as steroids, such as prednisone, to reduce nerve inflammation during MS flares. People with MS are also helped by physical therapy and medications to reduce fatigue.
Unlike MS, fibromyalgia isn’t a progressive disease and so it won’t damage your muscles or organs. But there is a connection between MS and fibromyalgia. “Any time patients have an autoimmune disease, there is a chance that they could develop fibromyalgia because of the stress and the chronic pain that comes from the autoimmune disease,” Dr. Kahlenberg explains. “Those things can reprogram the central nervous system, and crank up that pain volume receptor, so that even if we get the inflammation in their joints and muscles under control, the volume receptor can remain high.”
In other words, if you have an MS diagnosis, there’s a chance you can also have fibro along with it.
3. Rheumatoid Arthritis
Like many of the conditions mixed up with fibro, rheumatoid arthritis is an autoimmune disorder. It involves inflammation in the lining of your joints, called the synovium. It typically starts in the small joints in the hands and feet, though the body-wide inflammation in RA can also affect other parts of your body, including the skin, eyes, heart, lungs, and more.
And like patients with fibromyalgia, people with RA often have fatigue, weakness, and constant pain. And though the pain is in the joints, it can be tough to tell where specifically where it’s coming from when you ache all over.
But with RA you will have stiff joints — and that’s a key difference from fibromyalgia, according to Dr. Morris. “Patients with inflammatory diseases often are stiff for hours, while fibromyalgia patients usually can loosen up with 30 to 40 minutes,” he notes. Plus, there is swelling in the joints with RA, which isn’t the case for those with fibromyalgia, whose pain symptoms are more in the muscles, he adds.
Doctors will rule out rheumatoid arthritis by examining your bloodwork, screening for such blood proteins as rheumatoid factors and anti-CCPs, among other inflammatory markers. You may also have X-rays that show any damage to the joints (though this “radiographic damage” may not show up in the early stages of RA).
Left untreated, rheumatoid arthritis can deform the joints in your hands and feet and elsewhere and increase your risk for heart problems and lung disease. Luckily, treatments exist for even serious cases. Many patients take disease-modifying antirheumatic drugs, including biologics, along with low-dose steroids or pain relievers and find relief from the pain and swelling.
4. Polymyalgia Rheumatica
Polymyalgia rheumatica (PMR) is an inflammatory disease that causes widespread pain in the joints and muscles. It tends to occur later in life, typically first occurring in people over the age of 55, says Dr. Morris. That’s one key difference from fibro: Fibromyalgia patients tend to be a decade or two younger when they’re diagnosed. But some PMR symptoms can overlap with fibro, especially the widespread achiness and interrupted sleep.
There are other differences between fibro and polymyalgia rheumatica: PMR patients have prolonged morning stiffness, which gets worse from lack of activity, and have pain especially in the shoulders, neck, and arms, which inhibits range of motion. “Women with PMR often report problems fixing their hair due to shoulder muscle symptoms,” Dr. Morris notes.
PMR can be hard to diagnose. Doctors look for abnormal inflammatory markers (especially C-reactive protein) in blood tests. But sometimes the inflammatory markers appear normal, as they do in fibromyalgia patients.
That’s why Dr. Morris finds the tender points criteria useful when he is considering fibromyalgia. “There are an awful lot of patients who do have the tenderness in those localized areas. I don’t exclude the diagnosis of fibromyalgia if they don’t have the tender points, but it can help to support it,” he says.
PMR patients can get some relief with low-dose corticosteroids like prednisone as well as ibuprofen and other non-steroidal anti-inflammatory over-the-counter drugs.
5. Axial Spondyloarthritis
Back pain is a hallmark feature in this inflammatory type of arthritis that affects the vertebrate in your spine and the area where your spine meets the pelvis (sacroiliac joints).
AxSpA is often divided into two categories. Radiographic AxSpA (which is often called ankylosing spondylitis), means that evidence of joint damage is visible on X-rays. Non-radiographic AxSpA (nr-AxSpA) is essentially the same condition, but without joint damage being visible on X-rays.
Some symptoms of AxSpA can overlap with fibromyalgia — fatigue, lower back pain, jaw pain, and GI issues — but there are other symptoms that are more unique to AxSpA than to fibro. Chief among them are prolonged morning stiffness, says Dr. Morris — AxSpA pain gets worse when you sit still for long periods of time and improves when you’re more active. You may also have a fever and inflamed eyes, too.
Another complicating factor with fibro vs. AxSpA is sex: Fibro is much more common in women than in men, and ankylosing spondylitis is commonly — and mistakenly — thought of as a “man’s disease,” even though newer research suggests it occurs much more in women than previously thought. However, doctors may not necessarily suspect AxSpA in female patients, especially if they do not show damage to their joints on X-rays.
In fact, women are more likely to have non-radiographic axial spondyloarthritis than ankylosing spondylitis, and nr-AxSpA doesn’t show up on X-rays, though it’s possible to see some early changes on MRI. A thorough history, including questions about whether your back pain is inflammatory or mechanical, and full musculoskeletal physical examination are important to help doctors differentiate between fibro and AxSpA. Doctors must look at the joints, muscles, and range of motion.
6. Thyroid Disease
When you have generalized aches, exhaustion, and interrupted sleep you could have a number of conditions that don’t involve your muscles or joints. Some of these can be ruled out with a blood test.
Thyroid disorders top this list, especially hypothyroidism, which is when the thyroid doesn’t produce enough hormones. This causes some symptoms that can mimic fibromyalgia, including memory loss, constipation, and muscle weakness. That’s why Dr. Morris always tests for elevated levels of thyroid-stimulating hormone, a sign of hypothyroidism, in the patients who’ve been diagnosed with fibromyalgia by their primary doctors — and he’s found at few cases where there was an underlying thyroid condition as well.
7. Diabetes
Dr. Morris also checks glucose levels in blood and urine, in case people have an undiagnosed case of type 2 diabetes, which means their bodies can’t regulate blood sugar (glucose). Type 2 diabetes can produce general achiness and fatigue that mimic fibromyalgia, he says. But unlike fibro, the condition can lead to serious complications, including strokes, glaucoma, and heart disease, which is why it’s super-important to catch and treat it. Diabetes is easily diagnosed based on the levels of sugar in your blood or urine.
8. Anemia
Feeling tired is also a hallmark of anemia, which occurs when your body does not produce enough healthy red blood cells to carry the oxygen you need. If you’re anemic, you’ll also be weak and have headaches, just as you would with fibromyalgia, though you may not have pain or tingling in your muscles. The most common form of anemia is due to a lack of iron, but inflammation (say, from RA) can also cause anemia as can blood disorders and cancers. That’s why providers check red blood counts as they narrow their diagnosis.
9. Chronic Fatigue Syndrome
Think of chronic fatigue syndrome and fibromyalgia as flip sides of almost identical chronic conditions. Patients with CFS have many similar symptoms as those with fibro — brain fog, constant exhaustion, headaches, and poor sleep. And like fibromyalgia, women are much more likely to have CFS than men.
But there are differences between them. People with chronic fatigue have enlarged lymph nodes and sometimes a sore throat. And most importantly, the fatigue is more overpowering than the pain (the reverse is true in fibromyalgia).
Doctors aren’t exactly sure what causes chronic fatigue syndrome, though some think its origins could be viral — from the flu, say, or the virus that causes mononucleosis. But your provider will arrive at a diagnosis of CFS in a similar way to that of fibromyalgia, by excluding other conditions through careful sleuthing and tests.
Treatment can be tricky too. Sometimes even the gentlest workouts can make CFS symptoms worse (while they can be beneficial for patients with fibro, especially meditative exercise like tai chi, says Dr. Kahlenberg). Cognitive behavior therapy can help manage chronic pain, as can antidepressants, since CFS patients also have depression (understandably).
Getting to the Bottom of Fibromyalgia — or a Different Diagnosis
So how can you be sure you really have fibromyalgia? First, be sure your provider runs labs, gets a thorough medical history, including sleep (to rule out sleep apnea), and does a top-to-toe physical exam, says Dr. Morris. “We examine and look at the muscles and the joints and see if and where they’re tender. Do they have good range of motion? Do they have good muscle strength? Those are some of the things that we look for,” he explains.
Then your provider should ask questions like these: Is your pain and fatigue concentrated in the muscles or the joints? Does your pain get better or worse with activity?
While you don’t have to meet the tender points criteria, a doctor will probably follow these general guidelines to see whether you could have fibromyalgia.
You too should ask questions, says Dr. Kahlenberg: “‘Is there any evidence of inflammation?’ ‘Do I have evidence of any other autoimmune disease?’ ‘Could there be any other reason for my pain?’ I think an honest conversation with the doctor to say, ‘Why do you think this versus this,’ is a reasonable thing. If you don’t get answers that are helpful, then seek a second opinion at that point.”