Rheumatoid arthritis (RA) is a chronic inflammatory condition that causes painful swelling of the joints. If it isn’t treated, over time the disease can permanently damage your joints and cause many other health issues. That’s why it’s important to diagnose and begin taking care of RA as soon as possible. Early intervention can prevent long-term disability and other life-altering complications.
If your doctor suspects you have RA, to begin the diagnostic process, they will take your personal and family medical history, perform a physical exam, and order a number of lab tests. One of those tests will be for an autoantibody called rheumatoid factor (RF).
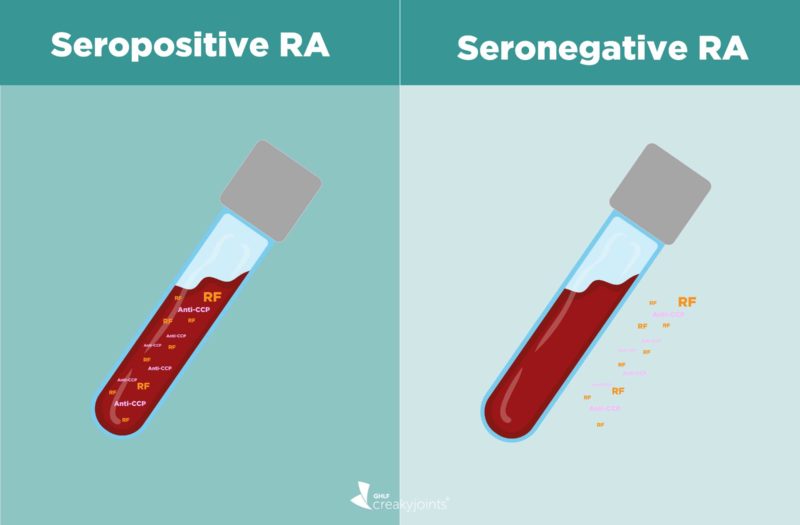
Many people with RA will test positive for rheumatoid factor in their blood. When you test positive for rheumatoid factor — and/or another autoantibody called anti-cyclic citrullinated protein (anti-CCP) — you are considered to have “seropositive rheumatoid arthritis.”
Some people with RA will have negative rheumatoid factor and negative anti-CCP. These patients are considered to have “seronegative rheumatoid arthritis.” For these patients, confirming an RA diagnosis will depend on other criteria. What’s more, once you are diagnosed, it may mean a different disease course — as well as some complicated feelings about your condition.
Here’s what you need to know about rheumatoid arthritis with negative rheumatoid factor.
The Connection Between Rheumatoid Factor and Rheumatoid Arthritis
Autoantibodies are proteins produced by your immune system. Rheumatoid factor is a kind of autoantibody.
When your rheumatoid factor levels are high, you may have an autoimmune disease, such as RA or Sjögren’s syndrome — or you may have another condition entirely. Among many other illnesses, elevated RF levels are associated with hepatitis C, leukemia, and endocarditis. Sometimes, even healthy older people have higher levels of rheumatoid factor.
Testing for rheumatoid factor can help diagnose RA, although it is just one part of a larger picture; there are many other criteria involved.
“Laboratory testing is confirmatory,” explains Jonathan Kay, MD, professor of medicine and population & quantitative health sciences and the Timothy S. and Elaine L. Peterson Chair in Rheumatology at the University of Massachusetts Medical School in Worcester. “It adds to the diagnosis, but by itself does not make the diagnosis of rheumatoid arthritis.”
When you are tested for rheumatoid factor, you will also be tested for anti-CCP (sometimes also called ACPA). Like the RF test, it does not confirm rheumatoid arthritis by itself, but helps to build a case for diagnosis.
What Does It Mean If My Rheumatoid Factor Is Negative?
While the percentage of people with seronegative RA has been estimated to be around 30 percent, a February 2020 study in the Annals of Rheumatic Diseases suggests that the trend has changed over the years, with more RA patients having the seronegative kind.
Researchers found that between 40 and 60 percent of people diagnosed with rheumatoid arthritis test positive for rheumatoid factor. The rest of RA patients have negative rheumatoid factor. Along similar lines, about half of people who meet the criteria for RA test positive for anti-CCP. That means between about half of rheumatoid arthritis patients test negative for anti-CCP.
Though there are exceptions, people who have symptoms characteristic of rheumatoid arthritis and who test positive for anti-CCP will almost certainly be diagnosed with the disease. Unlike positive rheumatoid factor — which is present in a number of different conditions — anti-CCP is very specific to rheumatoid arthritis.
If you test positive for rheumatoid factor or anti-CCP and are diagnosed with rheumatoid arthritis, this is referred to as seropositive RA. If you have negative rheumatoid factor and negative anti-CCP and are diagnosed with rheumatoid arthritis, it is called seronegative RA.
Occasionally, seronegative RA patients may develop antibodies and become seropositive at a later date — but this does not occur in most cases.
What Is the Normal Range for Rheumatoid Factor?
Though there is some variation depending on the lab, a normal level of rheumatoid factor is typically considered to be less than 15 or 20 IU/mL.
A number above that is considered to be abnormal, and means you are positive for rheumatoid factor. Generally speaking, the higher the rheumatoid factor, the more severe your disease may be.
Can You Still Have RA and Be Negative for Rheumatoid Factor?
If you have negative rheumatoid factor and test negative for anti-CCP, but other signs strongly point to RA, a rheumatologist can still diagnose you with rheumatoid arthritis. In this situation, Dr. Kay explains, “the diagnosis is based primarily on the patient’s description of their symptoms, their functional limitations — such as ability or inability to perform duties of daily living — and their physical examination revealing evidence of joint swelling and tenderness in a distribution characteristic of rheumatoid arthritis.”
Imaging can help confirm a diagnosis, as well. If joint erosion typical of rheumatoid arthritis shows up on an X-ray or ultrasound, it bolsters the case for RA.
Your doctor will also want to rule out the possibility of other disorders that may resemble RA. These conditions include, but are not limited to:
- Psoriatic arthritis
- Viral infections, such as parvovirus B19 or hepatitis B or C
- Gout
- Pseudogout
If, after satisfying these criteria, you are diagnosed with seronegative RA, your rheumatologist may revisit the diagnosis later on to make sure another condition doesn’t better fit your symptoms. For example, if you eventually develop scaly patches of skin called psoriatic plaques, you may actually have psoriatic arthritis instead of RA.
“You want to make sure there wasn’t a mislabeling or misdiagnosis,” explains Tuhina Neogi, MD, PhD, professor of medicine and epidemiology at Boston University Schools of Medicine and Public Health and chief of rheumatology at Boston Medical Center. “Medicine isn’t black and white,” she adds. “Sometimes there’s some gray and we don’t necessarily always have a definitive answer.”
Understanding Rheumatoid Arthritis with Negative Rheumatoid Factor
Though there are many exceptions, it’s historically thought that seropositive RA patients are at risk for more severe disease with more complications than seronegative RA patients.
“Traditionally it is said that seropositive rheumatoid arthritis has a more aggressive course with more joint destruction, formation of rheumatoid nodules, and perhaps more systemic involvement,” says Dr. Kay. “Traditionally, seronegative rheumatoid arthritis has had a less aggressive course.”
However, that does NOT mean that seronegative rheumatoid arthritis requires less serious treatment or attention. In fact, recent research has suggested that seronegative patients should be treated as aggressively as those who are seropositive.
Treatment for Rheumatoid Arthritis with Negative Rheumatoid Factor
Whether you have seropositive RA or seronegative RA, your rheumatologist will consider your individual situation when they develop your treatment plan. Your therapies will depend on your level of disease activity, your assessment of how you’re doing, and your physician’s assessment of how you’re doing, says Dr Neogi. “It is those types of assessments that guide therapy and when therapy needs to be escalated or changed,” she explains.
As for treatments themselves, there are very few differences in treatment options for seronegative RA patients — with some exceptions: rituximab (Rituxan). A biologic drug given via infusion, rituximab is prescribed to reduce symptoms when patients haven’t responded to other RA medications. “Analysis of clinical trials of rituximab have suggested that rituximab is less effective in patients who are seronegative,” says Dr. Kay. Similarly, the biologic medication abatacept (Orencia) might be more effective on seropositive RA patients than on those who are seronegative.
Most importantly, whatever your situation, it’s key to get an accurate diagnosis and start treatment in the first place. And the sooner you get started, the better off you’ll be, explains Dr. Kay. “With early initiation of effective therapy,” he says, “disease activity is often suppressed, regardless of the presence or absence or rheumatoid factor.”
Be a More Proactive Patient with ArthritisPower
Join CreakyJoints’ patient-centered research registry to track your symptoms, disease activity, and medications — and share with your doctor. Learn more and sign up here.
Keep Reading
Alten R, et al. Baseline autoantibodies preferentially impact abatacept efficacy in patients with rheumatoid arthritis who are biologic naïve: 6-month results from a real-world, international, prospective study. RMD Open. January 2017. doi: http://dx.doi.org/10.1136/rmdopen-2016-000345.
Autoantibodies. Lab Tests Online. https://labtestsonline.org/tests/autoantibodies.
Interview with Jonathan Kay, MD, professor of medicine and population & quantitative health sciences and the Timothy S. and Elaine L. Peterson Chair in Rheumatology at the University of Massachusetts Medical School in Worcester
Interview with Tuhina Neogi, MD, PhD, professor of medicine and epidemiology at Boston University Schools of Medicine and Public Health, and chief of rheumatology at Boston Medical Center
Myasoedova E., et al. Is the epidemiology of rheumatoid arthritis changing? Results from a population-based incidence study, 1985–2014. Annals of the Rheumatic Diseases. February 2020. doi: http://dx.doi.org/10.1136/annrheumdis-2019-216694.
Rituximab (Rituxan and MabThera). American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Treatments/Rituximab-Rituxan-MabThera.
Rheumatoid Arthritis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/diagnosis-treatment/drc-20353653.
Rheumatoid Arthritis (RA) Factor. LabCorp. https://www.labcorp.com/tests/006502/rheumatoid-arthritis-ra-factor.
Rheumatoid Factor. Medline Plus. U.S. National Library of Medicine. https://medlineplus.gov/ency/article/003548.htm.
Rheumatoid Factor. Medscape. https://emedicine.medscape.com/article/2087091-overview#a2.
Seropositive & seronegative. National Rheumatoid Arthritis Society. https://www.nras.org.uk/seropositive-seronegative.
Seropositive RA: What are the Facts About This Type of RA? Rheumatoid Arthritis.org. https://www.rheumatoidarthritis.org/ra/types/seropositive.
van de Laar MAF. Chapter 14 Rheumatoid Factors. Measuring Immunity. 2005. doi: https://doi.org/10.1016/B978-012455900-4/50276-2.