If you have high cholesterol or high blood pressure, your doctor may put you on medication to lower your cholesterol or blood pressure and tinker with the dosage or specific type of medication until you hit the ideal number. While managing rheumatoid arthritis is theoretically similar — you and your rheumatologist decide on a treatment regimen and then monitor how those medications are affecting your disease — the target can seem much less straightforward.
A main reason is that monitoring rheumatoid arthritis disease activity is more complex than simply measuring cholesterol or blood pressure. Doctors use different disease activity scores — which combine such factors as patient symptoms, physical exam results, blood tests for signs of inflammation, and surveys about how patients handle different daily activities and physical functions — to assess how well controlled RA disease activity is.
If RA disease activity is moderate or high, guidelines state that patients and doctors should consider whether a treatment is warranted to help patients achieve low disease activity or remission. This is called a treat-to-target approach: treating RA in order to reach a target that will allow patients to feel as healthy and functional as possible as well as prevent long-term damage and disease progression.
However, recent data published in the journal Arthritis Research & Therapy suggests that this process isn’t always working as it should.
In the study, whose initial findings were shared at the 2018 European Congress of Rheumatology meeting, researchers surveyed 249 rheumatoid arthritis patients through the ArthritisPower research registry, which is a partnership of the CreakyJoints arthritis patient community, researchers at the University of Alabama at Birmingham, and the Global Healthy Living Foundation (GHLF).
The main goal of the study was to identify factors that people with RA believed had influenced their physician’s treatment decisions. Study participants completed questions about their pain, fatigue, sleep disturbance, and physical function as well as a survey called the RAPID3, which is a patient-reported measure of rheumatoid arthritis disease activity. Participants also completed a survey about barriers to treatment optimization.
Here is what we learned from the results.
Most Patients in High Disease Activity Are Not Offered a Treatment Change
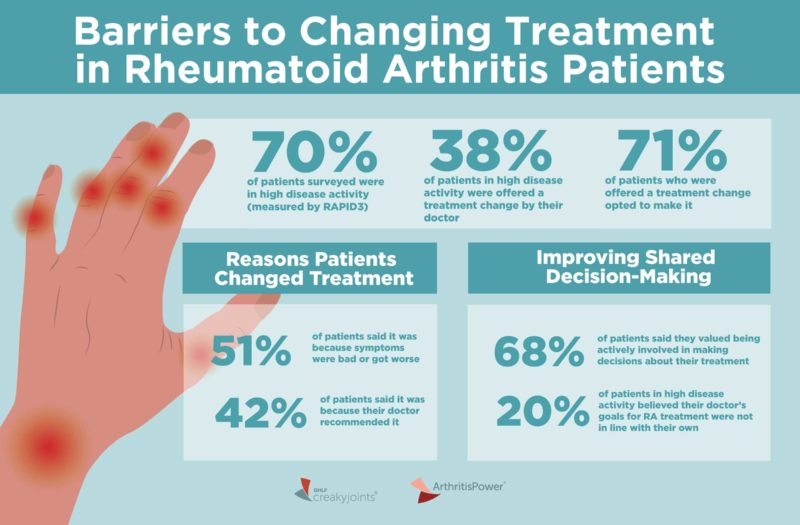
Of the 249 patients surveyed, the majority (70 percent) were considered to be in high disease activity based on their RAPID3 result. Of patients in high disease activity, only about one-third (38 percent) were offered a treatment change at their most recent visit with their rheumatologist.
The researchers then did a sub-analysis of patients who had persistently high disease activity over the past 12 months — perhaps they would report higher rates of being offered a treatment change since their disease activity was not improving over time? But the results were consistent. Only 39 percent of these patients said they were offered a treatment change at their last visit. This demonstrates that the failure of physicians to offer a treatment change was not simply related to short-term worsening (flare) of RA, the study authors wrote.
Patients Defer Decisions About Treatment Change to Their Provider
When RA patients were offered a treatment change, they tended to accept it: 71 percent of people in high disease activity and who were offered a treatment change opted to make it.
Among those who opted to intensify their treatment, 51 percent said that it was because their symptoms were still bad or had gotten worse and 42 percent said that their doctor recommended the change (participants could select all responses that applied to them).
Among those who opted to de-escalate treatment (which may be recommended to patients who are consistently remaining in low disease activity or remission), 60 percent said it was because their doctor recommended the change. (By comparison, only 27 percent said it was due to side effects.)
Among people who did not make any changes to their treatment, the most common reason (66 percent) for sticking with it was their rheumatologist’s satisfaction with the current therapy.
Patients Want to Be Actively Involved in Treatment Decisions, But May Need More Support to Do So
The majority of participants in high disease activity (68 percent) reported that they valued being actively involved in making decisions about their treatment.
The majority of participants with high disease activity strongly agreed or agreed (81 percent) that they trusted their doctor had recommended the best RA treatment for them; however, when replying to a different statement, 20 percent of participants in high disease activity strongly agreed or agreed that they believed their doctor’s goals for RA treatment were not in line with their own.
“I think what this discrepancy show us is that while patients believe that their doctor has their best interests in mind when recommending treatment options, patients may not always be having a conversation with their doctor about what their treatment goals really look like,” says study lead author Kelly Gavigan, MPH, manager of research and data science at the Global Healthy Living Foundation.
For example, a provider might be focused on making sure a patient’s lab results are normal and that their swollen/tender joint count is low, while a patient might just want to be able to walk their dog around the block twice a day with no pain.
“If patients can be more detailed and specific with their provider about how they hope their treatment will impact their daily function and RA symptoms, it can promote shared decision-making toward optimal treatment that both patients and providers can perceive as helping to control the disease,” says Gavigan.
Indeed, the concept of shared decision-making is important in the relationship between rheumatologists and patients. In this process, your doctor should describe benefits and risks of different treatment options (in this case, escalating or changing therapy compared with staying on a current regimen), you express your preferences, and together you decide on a path forward.
“But based on this survey data, we may need to find more ways to activate and educate patients to help them understand when they are in high disease activity, what that means for their short- and long-term health, and when it might be appropriate to talk to their doctor about a treatment change,” says study co-author W. Benjamin Nowell, PhD, PhD, director of Patient-Centered Research at the Global Healthy Living Foundation.
“There are many reasons patients may not broach this subject with the doctor, which this study didn’t specifically examine,” says Gavigan.
Patients may assume that if their doctor doesn’t bring up the idea of changing treatment, then they shouldn’t either. They may fear that switching to something new could be less effective than what they’re currently taking or introduce side effects. They may adjust to symptoms like pain and fatigue and assume that they are just part of living with rheumatoid arthritis.
But as more treatment options become approved for RA — each with different mechanisms of action — and as we learn more about precision medicine for RA patients, personalizing therapy to achieve maximum symptom relief will be the future and the norm for RA treatment.
“We need to empower RA patients who are experiencing notable pain, fatigue, and impacts on physical and daily function to bring this up with their doctor and talk about possible solutions that can help them feel better,” says Dr. Nowell.
This study was sponsored by UCB, which is a corporate sponsor of the Global Healthy Living Foundation.
Found This Study Interesting? Get Involved
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
Keep Reading
Gavigan K, et al. Barriers to treatment optimization and achievement of patients’ goals: perspectives from people living with rheumatoid arthritis enrolled in the ArthritisPower registry. Arthritis Research & Therapy. January 2020. doi: https://doi.org/10.1186/s13075-019-2076-7.