Psoriatic arthritis (PsA) is a complex and often frustrating type of inflammatory arthritis that impacts each patient differently. PsA is known to cause swelling, stiffness, redness, pain, and damage to the skin, nails, joints, and more. While it has the perception of being similar to rheumatoid arthritis but with skin involvement from psoriasis, in reality psoriatic arthritis is a completely distinct disease with its own risk factors, set of symptoms, and unique treatment options.
The majority of PsA patients already have psoriasis when they are diagnosed with PsA; it typically develops within five to 12 years of a psoriasis diagnosis. However, roughly 10 percent to 15 percent of people get joint pain symptoms before psoriasis skin plaques show up, explains Dafna D. Gladman, MD, FRCPC, professor of medicine at the University of Toronto, senior scientist at the Krembil Research Institute, and deputy director at the Centre for Prognosis Studies in The Rheumatic Diseases.
When it comes to psoriatic arthritis, no two patients are alike. Some individuals with PsA may have only peripheral joint disease (in which the hands, wrists, and knees are affected by joint symptoms), while others may have only spine involvement. Still, other people may have both, notes Brett Smith, DO, a rheumatologist at Blount Memorial Hospital in Alcoa, Tennessee.
“It can be difficult to fully assemble the puzzle and provide a formal diagnosis at times,” Dr. Smith says, “however, once a diagnosis is made, many of these symptoms or disorders respond to similar treatments.”
The most effective way to get your psoriatic arthritis under control is by working together with your rheumatologist to find the right combination of medications — and understanding the types and domains of psoriatic arthritis can help you do just that.
The 5 Types of Psoriatic Arthritis
There are five main types of psoriatic arthritis, categorized by the type of joint impacted. People can have one type initially only to develop another type later on.
Asymmetric oligoarthritis
Also known as asymmetric psoriatic arthritis, this type of PsA typically impacts less than five small or large joints in your body. It is called “asymmetrical” because the joint symptoms like pain and redness don’t occur on both sides of your body. You can have pain in the right knee but not in the left, for example. Roughly 35 percent of people with psoriatic arthritis have asymmetric oligoarthritis.
Symmetric polyarthritis
As the name applies, “symmetric” polyarthritis affects five or more joints on both sides of your body (e.g., the right and left elbows), similar to the symptoms of rheumatoid arthritis. This is the most common type of PsA, occurring in roughly half of people with the condition.
Distal arthritis
This type of PsA impacts the end joints of your fingers and toes (the distal interphalangeal joints), and can cause nail changes like spotting, pitting, or separating from the nail bed. Less than 20 percent of people with PsA have distal arthritis alone; it often occurs alongside other kinds of psoriatic arthritis.
Arthritis mutilans
This severe type of psoriatic arthritis can deform and destroy the joints in your fingers, hands, wrists, and feet. Arthritis mutilans prevent your bone cells from breaking down and rebuilding, which can cause your fingers to look like the opening of opera glasses (“opera glass hand”) or like a telescope (“telescoping finger”). Other symptoms of arthritis mutilans include stretched, shiny, and wrinkled finger skin; stiffness and immobility of the joint due to fused together bones (ankyloses); and wearing down of joints and bone tissues in the feet and hands. Thanks to growing advancements in treatment for psoriatic arthritis, arthritis mutilans is rare, occurring in less than 5 percent of people with PsA.
Spondyloarthritis
Psoriatic arthritis is considered a type of spondyloarthritis, which is an umbrella term for different types of arthritis that have some traits in common. (Ankylosing spondylitis and non-radiographic axial spondyloarthritis are also types of spondyloarthritis, for example.) In spondyloarthrits, people experience inflammation in the joints of the spine, which can cause pain and stiffness in the neck, lower back, and sacroiliac joints (located on each side of your spine). If left untreated, the vertebrae in your spine can fuse together. Your hands, feet, legs, arms, and hips may also be impacted. Psoriatic arthritis with axial involvement is a distinct condition that is different from having ankylosing spondylitis and psoriasis at the same time, a new study found.
Are ‘Types’ of Psoriatic Arthritis Outdated?
However, while these five types of psoriatic arthritis describe different presentations of the disease — and you may read about them online while you’re researching PsA — many rheumatologists no longer use them to classify PsA in patients. “We’re starting to think of people more as a whole,” says Rebecca Haberman, MD, a rheumatologist at NYU Langone. “It’s not just your joints or just your skin — psoriatic arthritis can involve all and any parts of the body.”
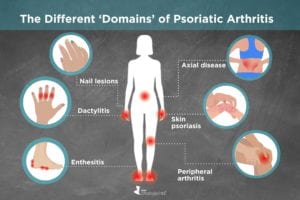
Why Psoriatic Arthritis ‘Domains’ Matter More
In order to better diagnose and treat patients, experts have identified six different domains (or manifestations) that people with PsA tend to experience:
- Peripheral arthritis
- Axial disease
- Enthesitis
- Dactylitis
- Skin psoriasis
- Nail lesions
Not everyone with psoriatic arthritis will experience all six domains. Each person can experience their own combination of domains that vary in severity. “Unfortunately, at this point, we can’t tell you who will progress to other domains or who will not,” says Dr. Haberman. It’s the mix and severity of these domains that influence how rheumatologists think about PsA treatment recommendations.
Peripheral arthritis
Peripheral arthritis tends to move from one joint to another, impacting the large joints of the arms and hands (elbows, wrists) and legs (knees, ankles). People with peripheral arthritis are more likely to develop inflamed toes or fingers and enthesitis (inflammation of the spot where tendons or ligaments attach to the bone). “Even though the swelling might go away, you can still be having underlying damage to the joint so you don’t want to ignore your symptoms,” warns Dr. Haberman.
Axial disease
Also known as spondylitis or spondyloarthropathy, axial arthritis causes pain and stiffness in the joints of the spine and sacroiliac joints (at the bottom of the back). Estimates regarding the presence of axial disease varies widely in PsA, ranging from 12 to 70 percent. “Patients with axial disease are more likely to have overall worse disease, including worse skin disease, yet researcher are not sure why,” says Dr. Haberman.
Enthesitis
Inflammation of the enthesis, which is where a tendon or ligament attaches to bone, impacts roughly half of people with psoriatic arthritis. While there are many areas where enthesis can occur, people with PsA often experience it in the Achilles tendon (heel) or the plantar fascia (bottom of feet) as well as the epicondyle (elbow).
“Why the heel/feet are more common is unknown but one theory is that enthesitis is brought on by microtrauma, and these areas might be more susceptible,” says Dr. Haberman.
Dactylitis
Dactylitis is the painful, red, and hot swelling of an entire digit — finger or toe — not just a knuckle within the finger or toe. It’s often called “sausage fingers,” because it can cause fingers to look like sausages. For many patients, dactylitis is their first symptom of PsA. “A patient who comes with dactylitis should clearly be evaluated for skin and nail disease,” says Dr. Gladman. “Sometimes the lesions are hidden in the scalp or around the anal area and are not clearly appreciated by the patient.”
Skin psoriasis
While some studies show that people with PsA tend to have worse skin disease than people with only psoriasis, you can develop PsA with just a very small area of psoriasis. In other cases, where on your body you get psoriasis may be indicative of your risk for going on to develop psoriatic arthritis. “Studies have shown that people with psoriasis that includes their scalp and nails may be at higher risk of developing PsA,” says Dr. Gladman. Skin psoriasis with PsA is different than psoriasis alone; it includes signs and symptoms in the joint, axial, and enthesis.
Nail lesions
Up to nearly 90 percent of people with psoriatic arthritis have nail involvement, including pitting of the nail, crumbling, spotted lunula (red spots in the white arch above the cuticle), and splinter hemorrhages (blood spots under the nail). This can include both fingernails and toenails, and it can be on one or all 20 nails, says Dr. Haberman.
How Psoriatic Arthritis Domains Impact Treatment Considerations
While there are clinical treatment guidelines from the American College of Rheumatology (ACR) and the National Psoriasis Foundation (NPF) for best managing the condition, your personal treatment plan will depend on how PsA is impacting your body as well as the severity of your symptoms.
In general, rheumatologists are advised to use a “treat-to-target” approach (treating patients as aggressively as needed to reach remission or low disease activity), which often includes prescribing tumor necrosis factor inhibitors (anti-TNF medications) or oral small molecule (OSM) drugs.
Beyond these guidelines, some medications have been found to work better for some domains than others. For example, conventional disease-modifying antirheumatic drugs (DMARDs) such as methotrexate (Trexall) and leflunomide (Arava) have been shown to work for the peripheral arthritis of PsA, but not for axial disease. These drugs are less effective, however, for enthesitis and dactylitis, notes Dr. Gladman.
Haberman adds that newer biologics called IL-17 inhibitors, like secukinumab (Cosentyx) and ixekizumab (Taltz) may be better when patients have little joint pain and a lot of skin involvement. Other types of biologics called IL-23 inhibitors, already approved for psoriasis, are currently being studied for psoriatic arthritis and will likely be available in coming years. One, guselkumab (Tremfya), had good results for PsA patients that were presented at the recent American College of Rheumatology/Association of Rheumatology Professionals Annual Meeting in Atlanta.
You can play your part in treating and managing psoriatic arthritis by becoming more aware of all the different parts of your body that PsA can affect.
“If you’re on medication and your skin is better but your back is hurting, you need to go back to your rheumatologist and tell them,” Dr. Haberman says. Don’t just blow off back pain as a pulled muscle or a sore elbow as “tennis elbow.” There are treatments that can be used to hit every part of your body impacted by your PsA.
Not Sure What’s Causing Your Pain?
Check out PainSpot, our new pain locator tool. Answer a few simple questions about what hurts and discover possible conditions that could be causing it. Start your PainSpot quiz.