“I always ‘wear a mask’ to hide my pain and how I’m feeling.”
“If I didn’t downplay my pain, I’d never talk about anything else.”
“No one really can comprehend what you’re dealing with. For those who do care, why worry them?”
“I put on the happy face for everyone and when I’m alone I’m the real me … I cry a lot.”
“Complaining won’t change anything and people get tired of hearing about it.”
These are just a smattering of the reactions from people in the CreakyJoints Facebook community when asked about how they talk about their chronic illness symptoms with others.
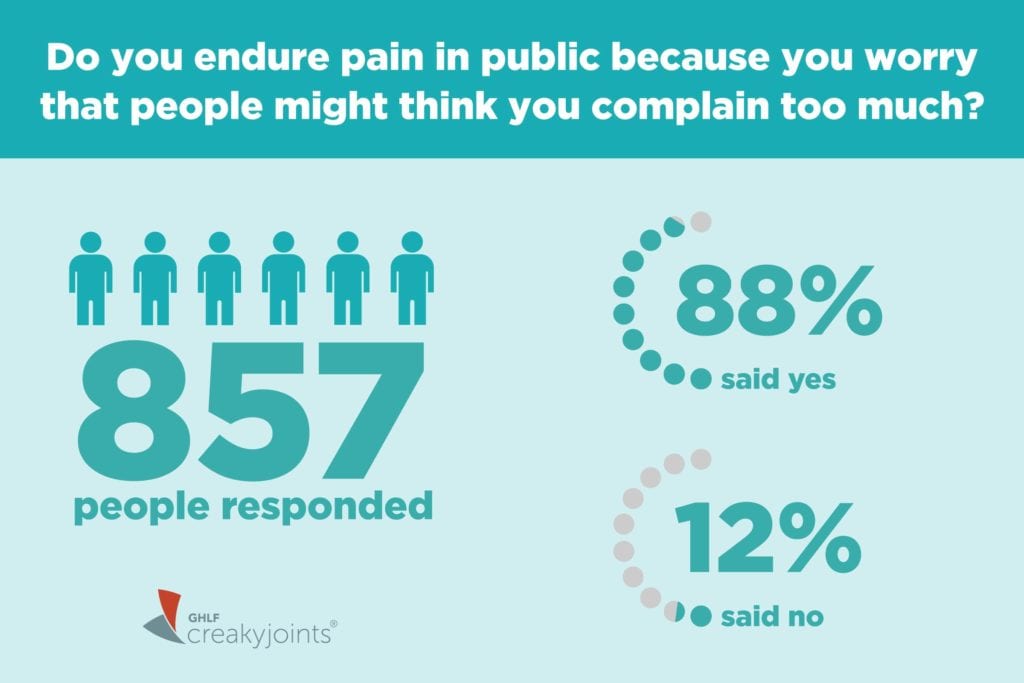
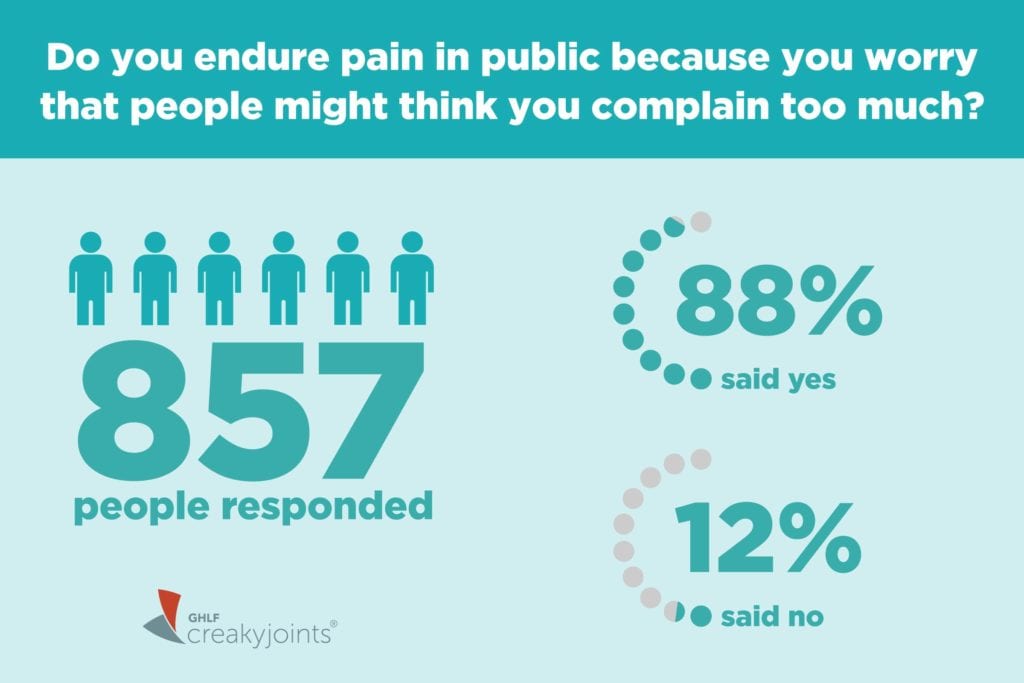
So the results of our latest ArthritisPower Community Poll are hardly surprising — but they’re still astounding. We asked people: “Do you endure pain or discomfort in public because you worry that people might think you complain too much?”
A remarkable 88 percent of the 857 respondents said yes. Only 12 percent said no.
“It’s a very common experience for people with chronic pain to fall into this situation with their social support group, where they do feel alienated by their symptoms,” says Jeffrey Wentzel, PhD, a clinical psychologist who sees patients in the New York City area.
Bottling Up Your Feelings Is Really Bad for Your Health
When you live with the constant ebb and flow of pain, fatigue, brain fog, or other symptoms of inflammatory arthritis, it’s natural to understand why you might limit your complaints. You don’t want to be perceived as a downer. You don’t think people really can ever understand how you feel. You don’t want to hear them minimize or downplay how you feel.
But when you keep your feelings about your pain — and for that matter, what it’s like to live with a chronic, lifelong illness that causes pain — bottled up inside, you might actually be making your pain worse.
“Feeling alone with something increases your anxiety about it and creates a state of hyper arousal,” says Dr. Wentzel. “When you’re in that state of hyper arousal, which has a lot to do with how isolated or not isolated you feel, you’re going to be much more sensitive to physical symptoms.” This can have a negative impact on your sleep, mood, and energy. You could even feel your pain more intensely as a result.
And yet, everyone’s been in situations where complaining falls on deaf ears, or for one reason or another, just seems to make you feel worse.
The key, Dr. Wentzel says, is to learn how to make your complaining about your pain more productive.
Don’t think of it as complaining. Think of it as being candid with the people in your life who genuinely care about you.
The Right Way to Complain About Pain
If you’re someone who avoids talking about how you feel because it feels pointless — that there’s nothing new to say, or that all you would do is talk about your pain — then “that tells me that there’s not something very productive happening in the way it’s being talked about,” says Dr. Wentzel. “A productive outcome is that you would feel better somehow. From my perspective, that means learning to talk about the emotions related to how you feel.”
In other words, talking about, say, how bad your back pain is today, or listing out the things you can’t do because of your pain is one thing. But it’s not likely to get as much empathy as would going to a deeper level where you discuss how the pain actually makes you feel.
“‘I feel helpless. I feel more alone, and this makes me sad.’ It’s kind of obvious but that more emotional way of talking about it is a way for other people to be engaged,” says Dr. Wentzel. It helps promote their empathy and understanding.
Here are more of his tips for being comfortable opening up to these emotions:
1. Start with some introspection. One of the first things Dr. Wentzel recommends to his patients is to start a journal. This can teach you how to talk more productively about your feelings. “I have them start with just the physical symptoms — just complain. Then in the second paragraph, how do you feel about hearing yourself say all that?”
This exercise, he says, helps you learn how to empathize with yourself. “If you can stop chasing away this thing that you resent having to deal with, if you’re empathizing with how it makes you feel, you are going to be much more receptive to someone else doing that too,” he says.
2. Identify your core people. “You really want to be talking about this in the right way with the right people,” says Dr. Wentzel. “There are going to be some people in your life you won’t feel comfortable telling how helpless this makes you feel. That’s just not a place you’re going to go with certain people.”
Think about who in your network — family, friends, coworkers, or even people in patient communities you meet online — can provide this kind of support for you. It might not be who you think, or it might change over time.
3. Find others with your condition. Even if you have the most amazing support system, there’s something to be said for speaking with people who have the same disease or symptoms as you. They instinctively get it. They may be more likely to know the right things to say, or not to say. They’ve been in your shoes.
Arthritis support groups, whether you find one that meets in person, or you communicate with people via social networks online, are a great outlet particularly while you’re learning how to talk productively about your pain, or if you’re worried about burning out your friends and family. (This woman’s Instagram memes help people with chronic pain feel less alone, for example.)
“A group of people who can share their experiences and are going to be more naturally empathic is so powerful and important,” says Dr. Wentzel.
4. Accept help. If you start discussing your pain with your friends and family, another common scenario you might encounter is that they want to help you. They might not know what to say, and they want to try to make things easier for you. This can be hard, but let them.
If people offer to help, don’t automatically say no. Maybe there are specific errands they can help with to give you a little more time to rest, such as driving your children to after-school activities. If you feel isolated and crave more companionship, tell them you’d love to meet for coffee or lunch more often.
Accepting help, in whatever form, will usually make you feel closer to that person. This creates a positive cycle, in which that person will tune in a little more and listen more carefully — “because it’s an emotional communication,” says Dr. Wentzel.
5. Know when you need professional support. While not everyone has the time or money to explore therapy, there are some people with chronic illness who would really benefit from professional counseling.
“If it feels like you’re so alone that you wouldn’t even know how to begin to talk about it with the people closest to you, or if you feel like you can’t even talk about your pain because it’s getting in the way of your closest relationships, that’s a recipe for things to get worse, and therapy is a good option to consider,” says Dr. Wentzel.
You should also be aware of common symptoms of depression — including changes in appetite; changes in sleep patterns; feeling sad, guilty, or helpless; not finding pleasure in activities you normally enjoy; or having thoughts of self-harm or suicide — and seek counseling if you experience them for more than two weeks.
Learn More About ArthritisPower
This question was one of our monthly ArthritisPower Community Questions, which offers ArthritisPower participants an opportunity to learn from each other and provide our research team insights.
If you’re diagnosed with RA or a musculoskeletal condition, you can participate in future polls like this, as well as research studies, by joining CreakyJoints’ patient research registry, ArthritisPower. As a patient-led, patient-centered initiative, our research team is committed to investigating research topics that matter most to you.





