This year is poised to be a big year for biosimilars, mainly because the period of exclusivity for Humira (adalimumab) has come to an end. The loss of exclusivity opens the door for adalimumab biosimilars to hit the market. The first one, Amjevita (adalimumab-atto), is already here as of January 31, and at least seven others are expected to follow soon.
The growth of biosimilars is good news for patients because it means more options will be available when you need to fill a prescription or go to a clinic for an infusion. It should also mean that you’ll save money, but that won’t necessarily be the case. A new report from the Patient Access & Affordability Project explains why.
The report was based on a roundtable discussion of health care experts, including Robert Popovian, PharmD, Chief Science Policy Officer at the Global Healthy Living Foundation. It is designed to highlight current trends, explain the benefits of biosimilars, and alert patients to the fact that they will likely miss out on the financial perks associated with biosimilars, at least in the short-term.
What Are Biosimilars?
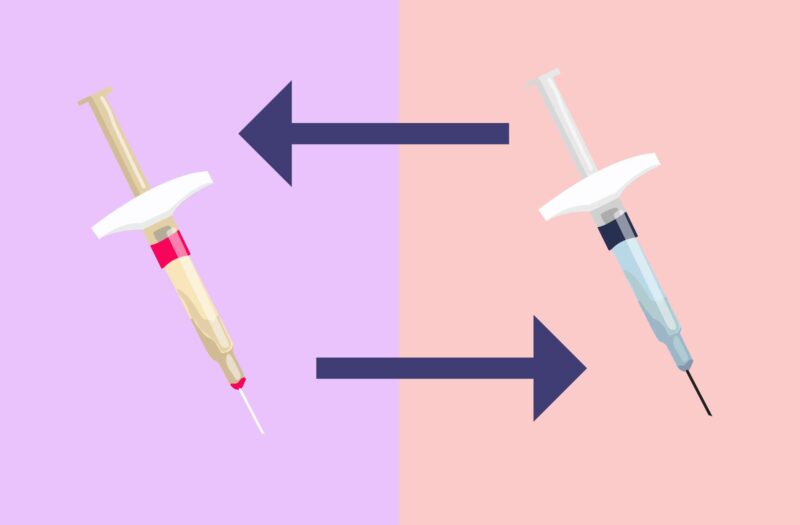
Biosimilars are essentially generic versions of biologic medications. Technically, they’re not the same as generic drugs because it’s impossible to reproduce a biologic drug exactly. Biologics — and the biosimilars that are meant to mimic them — are made from a complex process and entail the use of living cells. According to the Food and Drug Administration (FDA), biosimilars are “highly similar [to the original biologic they’re designed to copy] and have no clinically meaningful differences from an existing FDA-approved reference product.”
FDA-approved biosimilars “have been studied for a long time, work the same for your condition, and the safety and quality are the same,” says Sameer Awsare, MD, Associate Executive Director of the Permanete Medical Group, who participated in the Patient Access & Affordability Project roundtable. That means if you were used to taking, for instance, Remicade (infliximab) and you switch to a biosimilar of it such as Inflectra (infliximab-dyyb), you shouldn’t notice any difference in terms of how well it works for you. Dosing and potential side effects should also be identical.
Biosimilars aren’t easy to make, but their development cost is significantly less than developing a novel brand biologic from scratch, says Dr. Popovian. Moreover, their presence means that there will be competition in the marketplace, compelling drug manufacturers to lower prices to make their products more attractive to health insurance companies and other payers (like Medicare).
The use of biosimilars has already translated to savings of about $13 billion across the health care system, and that number could jump to $130 billion by 2025, according to the Biosimilars Council. The catch is that these savings often do not make it to patients.
Why Aren’t Patients Switching to a Biosimilar Saving Money?
The problem, Dr. Popovian explains, stems from the fact that a patient’s coinsurance or deductible for biologics self-administered at home (such as Humira or a biosimilar like Amjevita) is based on inflated retail prices. Pharmacy Benefit Management (PBM) and insurance companies negotiate deep discounts based on rebates with the biopharmaceutical manufacturers; unfortunately, those savings are not shared with the patients and are primarily hoarded as profit by PBMs and insurers.
Here’s how it works: Let’s say you fill a prescription for Humira, and the retail price is $500*. If you’re among the growing number of people with coinsurance (rather than a flat fee copay), you’ll pay a set percentage of that retail price after hitting your deductible for the year. If your coinsurance is 20 percent (and you’ve already hit your deductible), you’ll pay $100 when you get your prescription. But at the same time, your insurer might also be getting a rebate from the drug manufacturer — let’s call it $250. So your total cost of $100 was based on the inflated retail price, not the price that the PBM or insurer negotiated on your behalf.
The presence of biosimilars and the way the pharmacy benefit design is set up allows PBMs and insurers to leverage market competition and negotiate steeper rebates that are never passed back to the patient at the point of sale.
PBMs may sometimes pass back some of the savings to the insurer. Still, due to consolidation in the past years, the insurers and PBMs are the same; the savings or profiteering stays within the insuer/PBM conglomeration.
Ultimately, “It’s more lucrative for PBMs to maintain the formulary presence of a more expensive drug that they can negotiate higher rebates for,” says Dr. Popovian.
What You Can Do
Step one: Educate yourself about biosimilars. Listen to GHLF’s Breaking Down Biosimilars and Health Care Matters podcasts, download our Patient’s Guide to Understanding Biosimilars, and read the Patient Access & Affordability Project report.
Similarly, educate yourself about your pharmacy benefits. You may or may not have a choice between a biologic and a biosimilar, and even if you do, you shouldn’t assume without checking that your cost for the biosimilar will be less — though it might be.
Patients who are part of Kaiser Permanente, which is a non-profit integrated health system that includes pharmacy benefits, will certainly see the savings right away by switching from a biologic to a biosimilar, says Dr. Awsare. “We don’t believe in rebates; we just lower the price,” he says, noting that when patients can’t afford medication it only drives up other costs, such as those related to hospitalizations. “There’s no benefit to us to keeping patients sick.”
Suppose your doctor or changes in your health plan nudge you toward using a biosimilar. In that case, that’s OK because these copycats are just as safe and effective as the biologics they originated from. But you should also see your out-of-pocket costs come down as a result. If that’s not happening — or, even worse, if your health care costs are going up — sharing your story may help patient advocates continue to push for legislative reform. Write us at HealthcareMatters@ghlf.org to let us know your experience.
*These numbers are just for illustrative purposes. The amount your insurance pays for a drug, the percent of your coinsurance, and the rebates negotiated for a particular product will all vary by insurance plan.
If you enjoyed reading this article, you’ll love what our video has to offer.
Interview with Robert Popovian, PharmD, Chief Science Policy Officer at the Global Healthy Living Foundation
Interview with Sameer Awsare, MD, Associate Executive Director of the Permanete Medical Group.
Patient Access & Affordability Project. Special Report: The Biosimilars Market in 2023: Important Trends and Milestones for Chronic Disease Patients. https://accessandaffordability.org/wp-content/uploads/2023/01/2023-BioSimilars-Report-FINAL-01242023.pdf.
U.S. Food & Drug Administration. Biological Product Definitions. https://www.fda.gov/files/drugs/published/Biological-Product-Definitions.pdf.