One of the main reasons people with arthritis visit the rheumatologist frequently — every three months is common among patients with inflammatory arthritis — is for doctors and patients to assess how arthritis patients are managing their disease. Typical check-ins may include a doctor’s physical exam and assessment as well as reviewing the results of blood tests and imaging tests.
What’s also critical at these visits is something arthritis researchers and doctors call PROs, or patient-reported outcomes. PROs are a patient’s own assessments of how arthritis affects daily tasks — including how you rank or define the difficulty of simple activities like getting in and out of your car or buttoning your shirt — and are a very important tool for measuring and monitoring your disease.
PROs are also important during clinical trials for medications or other treatments, as they can assess how different therapies affect patients and the symptoms that matter to them.
There are many different PRO measures and questionnaires doctors and researchers can use, but which symptoms are most important to patients? This is an important topic that the rheumatology community needs to know more about, so researchers, including those from our non-profit organization, the Global Healthy Living Foundation (GHLF), set out to study this.
“PRO measures are important indicators of disease activity, but as we learn more about the importance of their role in evaluating treatment effectiveness, we need to also learn more about the specific symptoms that patients find most important to track,” says study co-author Kelly Gavigan, MPH, manager of research and data science at GHLF.
In research presented at the 2019 American College of Rheumatology/Association of Rheumatology Professionals (ACR/ARP) Annual Meeting in Atlanta, researchers surveyed 253 patients through our ArthritisPower research registry with various self-reported conditions, including rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), systemic lupus erythematosus (SLE), osteoporosis (OP), osteoarthritis (OA), and fibromyalgia syndrome (FMS).
At the start of the study, patients could select up to 10 different symptoms they wanted to track via short health assessment questionnaires. Study participants would then go on to complete the assessments once a month for the next three months. The symptoms that patients could track included:
- Pain
- Physical Function
- Mental Health (including depression, anxiety, and anger)
- Fatigue
- Social Health
- Sexual Function
- Sleep Disturbance
- Duration of Morning Joint Stiffness
- RA Flare (for RA patients only)
On average, participants chose to track seven different symptoms at the start of the study.
The Symptoms that Matter Most to Patients
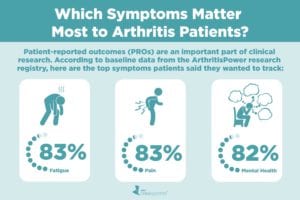
In evaluating the PROs that were most popular among study participants at baseline, three stood out:
- Fatigue: 83 percent of patients chose fatigue as a PRO they wanted to track.
- Pain: 83 percent of patients chose pain as a PRO they wanted to track.
- Mental health: 82 percent of patients chose mental health as a PRO they wanted to track. Within mental health, 54 percent of patients wanted to track depression and 44 percent of patients wanted to track anxiety.
Here is the percentage of patients who wanted to track other PROs in the study:
- Physical Function: 72 percent
- RA Flare: 70 percent (only offered to RA patients)
- Social Health: 67 percent
- Sleep Disturbance: 65 percent
- Duration of Morning Joint Stiffness: 57 percent
- Sexual Function: 11 percent
Putting a Spotlight on Mental Health
Study participants were also asked to share any self-reported comorbidities, or other diseases they have along with their arthritis diagnosis. The most common comorbidity was depression, reported by 51 percent of participants. This may partly explain why so many participants were interested in tracking aspects of their mental health.
National data show that depression and anxiety are common among people living with arthritis. According to a 2018 CDC report, 23 percent of people with arthritis reported symptoms of anxiety and 12 percent reported depression. These rates are likely even higher among specific populations of arthritis patients. For example, a 2019 study found that people with ankylosing spondylitis were twice as likely to have depression as people without AS. Other research has indicated that depression rates are higher among people with psoriatic arthritis than other rheumatologic conditions.
“Our research shows us that mental health is a top priority for patients and they do want to keep track of it,” says Gavigan. “But we know it can be challenging for some people to discuss mental health issues with their rheumatologist or other providers.”
In fact, other GHLF data suggest patients aren’t talking about their mental health with their rheumatologist. In a 2018 poll of ArthritisPower users, 59 percent of nearly 1,000 respondents said that their rheumatologist or primary care doctor does not ask about their mental health.
“We hope that being able to log and track mental health symptoms through ArthritisPower can facilitate these discussions and ensure that patients get the care and support they need to cope better with chronic illness,” Gavigan adds.
Fatigue: As Important as Pain
As many patients — 83 percent — reported wanting to track their fatigue as they did pain, which is important for rheumatology clinicians and researchers alike to know.
“We often hear from our arthritis patient community that fatigue is difficult to talk about with care providers,” says Seth Ginsberg, president and co-founder of CreakyJoints, which is part of GHLF. Patients report that doctors don’t always take their fatigue as seriously as other symptoms. What makes this even more challenging is that loved ones and caregivers also often struggle to understand the impact of fatigue on someone living with arthritis — that it’s more than just feeling tired. People who have fatigue from chronic illness are not “lazy” or “just need to get more sleep.” Fatigue is a physical manifestation of their disease, just like pain, stiffness, or swelling.
“The more patients can quantify difficult-to-discuss symptoms like fatigue, and mental health concerns, the more we as a rheumatology community can evaluate disease activity, treatment effectiveness, and overall health in a broader context that more fully takes into account patients’ complex experiences living with complicated, lifelong chronic diseases,” says W. Benjamin Nowell, PhD, director of Patient-Centered Research at GHLF.
Found This Study Interesting? Get Involved
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
Keep Reading
- A Patient’s Guide to Monitoring RA Disease Activity
- Arthritis and Depression: Understanding the Link
- Strategies for Coping with Fatigue from Chronic Illness