Fibromyalgia and lupus are both chronic diseases with no cure, can both cause some similar symptoms, and can both take a long time to get the right diagnosis. But fibromyalgia — often called fibro — and lupus are two very distinct health conditions with very different causes and treatments, despite having some features in common.
Lupus is an autoimmune disorder that involves widespread inflammation and impacts many organs throughout the body. Fibromyalgia a disorder that causes widespread chronic pain and tenderness. Unlike lupus, fibromyalgia is not an inflammatory or autoimmune disease.
Still, many signs and symptoms of fibromyalgia and lupus overlap and it’s not uncommon for fibromyalgia to be misdiagnosed as lupus, says rheumatologist George Stojan, MD, an assistant professor of medicine at Johns Hopkins University School of Medicine and co-director of the Johns Hopkins Lupus Center in Baltimore, Maryland. Both fibromyalgia and lupus can cause muscle/joint pain, brain fog, and fatigue. Both are also more likely to occur in younger and middle-aged women.
Interestingly, another factor that makes fibromyalgia and lupus difficult to differentiate from each other is that some people have both at the same time. “Having both lupus and fibromyalgia is extremely common,” says Dr. Stojan. “In our cohort here at Hopkins about 30 percent of lupus patients have fibromyalgia too.”
People with other rheumatic diseases such as rheumatoid arthritis, osteoarthritis, and axial spondyloarthritis are also at an increased risk of also having fibromyalgia.
Read more to learn about the different symptoms of fibromyalgia vs. lupus, how fibromyalgia and lupus are each diagnosed, and how treatments for fibromyalgia and lupus differ.
The Basics of Fibromyalgia
The U.S. Centers for Disease Control and Prevention (CDC) estimates that about 4 million American adults have fibromyalgia. While doctors don’t know what causes fibromyalgia, it is a disorder in which people often experience widespread chronic pain and sensitivity to touch, in addition to many other symptoms (more on this below).
Unlike lupus, fibromyalgia is not an autoimmune disease, which occurs when then body’s immune system mistakenly attacks your own cells and tissues. Fibromyalgia is not related to inflammation, nor is it a joint or muscle disorder caused by physical injury.
People at higher risk of fibromyalgia include women, the middle-aged, and those with certain diseases, including different types of arthritis, or a family history of fibro. While fibro can impair your quality of life, it doesn’t damage your tissues and organs, or cause medical problems like heart disease. It is not life-threatening.
Common Symptoms of Fibromyalgia
Widespread musculoskeletal pain all over the body
Fibro’s hallmark symptom is persistent pain in soft tissues and muscles all over the body. It may involve tender points, or areas of tenderness in specific parts of body. Frequently described as a deep ache, fibro pain may move around, persist for long periods, and disappear.
Fatigue
More than nine in 10 fibromyalgia patients experience exhaustion. Fatigue can be especially noticeable when you first wake up in the morning, even when you’ve gotten plenty of sleep; light activity can make pain and fatigue worse.
Cognitive issues
People with fibro can have difficulty concentrating or switching between tasks, frequently referred to as “fibro fog.”
Tension or migraine headache
More than half of patients with fibromyalgia have frequent headaches.
Weird body sensations
Some people with fibro report tingling, burning, numbness, or creepy-crawly sensations in both arms or legs.
Other symptoms
Fibromyalgia patients often also have irritable bowel symptoms, pelvic pain, and jaw/facial pain.
Read more here about fibromyalgia symptoms.
The Basics of Lupus
The Lupus Foundation estimates that 1.5 million people in America have a form of lupus. Lupus is an autoimmune disease that occurs when your immune system cells — which are supposed to protect the body from different germs — start treating normal, healthy cells like invaders, attacking them and causing flare-ups that can affect the joints, skin, heart, lungs, kidneys, and almost any other system in the body.
Women of childbearing age (between 15 and 44) are at the highest risk of developing lupus, according to the CDC; some 90 percent of people with lupus are women. People of color — particularly African Americans — are at a higher risk of lupus than white people are, and the disease tends to affect populations differently. Native American and black patients tend to have higher mortality rates than white patients, while Hispanic and Asian patients have a lower risk of lupus.
There are several types of lupus, but most people refer to the most common form: systemic lupus erythematosus, also known as SLE. About 70 percent of people with lupus have SLE, according to the Lupus Foundation of America. Lupus can cause a range of complications; some, such as heart disease and kidney disease, can be severe and even life-threatening without early and proper medical treatment. Regular medical care that utilizes an integrated team of specialists is important to help lupus patients avoid life-potentially serious complications.
Common Symptoms of Lupus
Painful, swollen joints
These are usually far from the center of your body, such as joints in the fingers, toes, ankles, wrists, knees, and elbows.
Swelling around the eyes and extremities
Kidney inflammation can cause fluid retention that can make ankles, feet, legs, hands, and sometimes eyelids feel puffy and swollen.
Unintentional weight loss (or sometimes gain due to swelling)
Unexplained weight loss — not due to dieting, other illness, or medication side effects — can be a sign of lupus. On the other hand, weight gain caused by fluid retention can also be a sign of the disease.
Rashes and skin lesions
The characteristic rash across the cheeks and nose (called a malar rash) is one of the most recognized symptoms of lupus, although a similar-looking rash can also occur in other skin issues. Another type of lupus skin issue is a discoid rash that causes raised, red, and scaly patches.
Sensitivity to sunlight and cold temperatures
Sun exposure can cause a lupus rash to develop or flare. People with lupus are also at risk of developing Raynaud’s, a condition in which the small blood vessels in the hands and feet suddenly constrict when exposed to cold or stress.
Other lupus symptoms include fever; neuropsychiatric issues such as depression, anxiety, seizures, or psychosis; brain fog; fatigue; headaches (including migraine-like attacks); mouth ulcers; kidney problems; and chest pain.
Read more here about lupus symptoms.
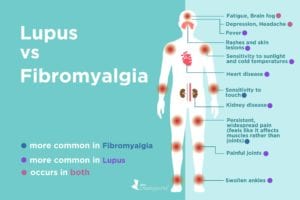
Symptoms that Lupus and Fibromyalgia Have in Common
- Pain
- Cognitive issues
- Fatigue
- Headaches
Key Ways Fibromyalgia and Lupus Are Different
Despite the similarities in some of the symptoms, there are a few clear differences doctors and patients should be on the lookout for, says Dr. Stojan.
1. The nature of fatigue: Fatigue is common during a lupus flare, but it will subside once the attack is over, says Dr. Stojan. In fibromyalgia, however, exhaustion is more chronic — it’s less likely to come and go.
2. The nature of pain: Although both fibromyalgia and lupus can cause muscle and joint pain, lupus pain persists until it’s treated, says Dr. Stojan. The pain of fibromyalgia comes and goes. “The transient quality of the symptoms is a reliable sign that pain is not related to lupus,” he says.
3. Whether skin is involved: Fibromyalgia doesn’t cause nose and/or mouth ulcers or rashes like lupus does, such as the typical “butterfly” rash on the cheeks and bridge of the nose that can pop up during a lupus flare.
4. Whether there is inflammation: In lupus, a patient’s immune system starts to attack organs and other body tissues, leading to widespread inflammation that will likely show up in lab tests or imaging, says Dr. Stojan. Fibromyalgia, on the other hand, does not cause inflammation.
Getting the Right Diagnosis
There are no definitive tests for either fibromyalgia or lupus, so differentiating between the two relies mostly on a thorough history of your symptoms, a physical exam, and sometimes blood tests or imaging to rule out other conditions. Read more here about how fibromyalgia is diagnosed.
Your doctor will ask you to describe your pain — and if they suspect fibromyalgia, may perform a “tenderness” test, pressing on several parts of your body to gauge where the tenderness is, and how severe it is.
Your doctor will likely also ask whether you experience fatigue, wake up tired every morning, or have trouble concentrating or experience brain fog — and for how long you’ve had these symptoms.
Your doctor may order some blood tests in order to rule out diseases that can cause fatigue, such as hypothyroidism type 2 diabetes. They may order blood tests to check for levels of inflammation in the body or for antibodies that could signal an autoimmune disease. One test ordered to help confirm or rule out lupus is the blood test for antinuclear antibodies (ANA). A positive test can be one sign of lupus, but it doesn’t necessarily mean you have it. “ANA is a very common marker people have in the blood. Almost one-third of people in the U.S. will test positive — and that alone doesn’t mean you have lupus,” Dr. Stojan says. However, most people who have lupus will have a positive test.
If you have a positive ANA test and other signs that point to lupus, your doctor may do additional antibody tests that help confirm or rule out the illness.
Your doctor may also order imaging tests like X-rays or MRIs to narrow down the cause of your symptoms. Neither fibromyalgia or lupus cause erosion in the joints (the way rheumatoid arthritis does) or visible inflammation of the lower back (the way axial spondyloarthritis does).
Treatment for Fibromyalgia vs. Lupus
Neither disease has a cure, but medication can treat symptoms and help prevent serious lupus complications. The medications used to treat lupus are very different from those used to treat fibromyalgia.
For fibro patients: Some drugs commonly used to treat depression, called antidepressants, may ease pain and fatigue; these include duloxetine (Cymbalta) and milnacipran (Savella). Anti-seizure medications, frequently prescribed to people with epilepsy, can also help manage pain in fibromyalgia. Among these, the FDA has specifically approved pregabalin (Lyrica) for the treatment of fibro.
For lupus patients: Many different types of medications can be used to treat lupus, including:
- Non-steroidal anti-inflammatory drugs (NSAIDs) to relieve pain and inflammation
- Hydroxychloroquine or chloroquine, a malaria drug that is also useful at treating lupus flares, joint pain, and skin rashes
- Glucocorticoids, or steroids, to relieve inflammation and treat flares
- Immunosuppressive medications, such as azathioprine, cyclophosphamide, methotrexate, mycophenalate mofetil
- Targeted biologics, such as rituximab (Rituxan) and belimumab (Benlysta), which reduce the activity of the immune system by targeting specific immune cells
- Other medications to help manage complications of lupus, including those for cholesterol, blood pressure, osteoporosis, and others
Patients with lupus and fibro can also benefit from healthy lifestyle practices, too, including:
- Exercise: Regular physical activity can help manage symptoms of fibro or lupus, and may improve mood, fitness and function. Swimming, walking, tai chi, and yoga are smart options. Exercise can be very important in helping people with lupus reduce their risk of cardiovascular disease complications. Consult a health care provider or physical therapist about a new exercise regimen, so it can be adapted to individual needs.
- Diet: Though there is no specific diet recommended for lupus or fibro, a healthy eating plan may boost your immune system, help manage co-existing conditions, and promote overall good health. Read more about a following a healthy diet for lupus and a healthy diet for fibromyalgia.
- Sleep: Getting adequate rest is vital for both conditions. It’s recommended that adults between ages 18 and 64 should aim for seven to nine hours nightly.
- Complementary practices: Some patients report that activities like meditation, acupuncture, deep breathing, and massage help them relax and ease symptoms.
While lupus and fibro may have some symptoms in common, they are ultimately distinct conditions with very different causes and treatments. Visiting a health care provider can help you get to the bottom of your symptoms quickly and begin the correct therapies. The faster you start, the faster you can start feeling better.