“Vegetable soup you make yourself, two pieces of fresh fruit per day, up to one avocado per day, up to two ounces of nuts per day — chewed well. Two to three servings per week of baked wild-caught fish, purified water, and non-caffeinated tea.”
The above is an excerpt of a highly prescriptive eating plan I was placed on by doctors in order to try to manage my various medical conditions, including ankylosing spondylitis and fibromyalgia. This was not the first time I’d tried drastically changing my diet in order to heal myself (or at least control my symptoms). I’d tried removing nightshade vegetables, cutting out caffeine, adding more caffeine, reducing my intake of meat, increasing my intake of meat, eliminating asparagus and soy, eating nothing sweet before 2 pm, and intermittent fasting.
If you live with chronic illness, then you’re likely no stranger to the variety of dietary changes and eating plans suggested by health care professionals, loved ones, and strangers alike. Doctors, family, and friends are quick to proclaim the success you will have and how much better you will feel if only you try this one thing. I once even had a complete stranger email me after seeing an article I’d written, suggesting I try eating nothing but sweet potatoes and romaine lettuce, and claiming he’d healed himself doing so.
Desperate to feel better, I was willing to try just about anything, and so I changed the way I ate over and over again. I wasn’t listening to my body but to what others were telling me would help me.
Feeling Like a Failure
For me, though, none of these changes were sustainable. In some cases, the difficulty of avoiding certain foods was too much. In other cases, the dietary changes didn’t seem to make a difference or even made me feel worse. Nearly always the restrictions I placed on my eating triggered a lot of emotions for me linked to my history with disordered eating, and sent me spiraling internally about my body image and weight. Oftentimes, I felt I was missing out, not just on foods but also on the social aspect that is so often tied to and connected to eating.
As such, I’d “fall off the wagon” of whatever dietary plan I was attempting, and I’d immediately grapple with guilt and feelings of unworthiness. I felt like I’d failed, not only at the change in my diet, but also like I’d failed myself. I’d beat myself up over not being able to maintain these changes, and felt like it was my fault I wasn’t getting better.
While the dietary plan above was not the first one I’d tried, it was my last. It simply was not sustainable for me. After I “failed” at the rigid plan my doctors had given me and went through another round of feeling guilt and shame, I realized that something needed to shift. I couldn’t go on like this. Not only was it not good for my mental health, but it felt like it may even be impacting my physical health too.
“Increased stress around foods is more likely to exacerbate chronic illness symptoms than the food itself,” Intuitive Eating Coach and Licensed Professional Therapist-Associate Lauren Hansen told me. And in my case, this seemed very much to be true.
What Is Intuitive Eating?
“Intuitive eating is a sustainable and realistic approach to eating that allows you to focus on creating habits that honor your body rather than punish it,” Registered Dietician Caitlin Mudd, RD, LDN, told me. It is based on 10 principles that help you tune into your own body’s cues. This takes the focus away from calorie intake, weight, and what foods you can’t eat.
Hansen defined intuitive easting as “attuning to your body’s needs from a place of care, connection, and joy.”
With intuitive eating, often abbreviated to IE, the focus isn’t on restricting foods, but really on listening to your own body and what it needs and wants. One of the basic beliefs is that our bodies know what we need and have the ability to cue us into that, and that if we listen to our bodies, we will be able to respect those needs and eat in ways that provide care for both our physical selves but also our emotional selves.
I first came across intuitive eating when I first started by body positivity journey. Although I didn’t try it until years later. I needed a sustainable and realistic way to care for my own body in a way that made sense for me, and all aspects of me.
How to Practice Intuitive Eating with Chronic Illness
Practicing IE while chronically ill can be a bit more complicated since certain foods can trigger symptoms and medications can also mask natural hunger cues.
When I began practicing intuitive eating, it was a total shift in mindset and practice. No longer was I viewing foods as bad or good, but just as foods. Instead of surrounding food and eating with judgment, I tried to neutralize it and remember the joy and pleasure that can be associated with food. Additionally, I really began to tune into what foods did and didn’t work for me.
For those with autoimmune issues, such as various forms of arthritis, intuitive eating is about “turning to what you lovingly need in that moment,” says Chelsea Sheridan, a certified Health Coach who specializes in autoimmunity. “If it’s a bowl of ice cream with your boo, enjoy it. If it’s an extra-large bowl of broccoli when you’re out for dinner — that may be all you need.”
Sheridan talked to me about not only paying close attention to what your body needs, but also the symptoms that may come up after you eat. “Acknowledge these symptoms — and take note of them for the future — and consider some tools that might help you get through the discomfort,” she says. “Eat when and what feels best and most supportive to your body…keep in mind these foods can change over time.”
What Intuitive Eating Has Taught Me
As I tune into my body and get to know better what it wants and needs, I find myself feeling freed from so many negative associations to food I’ve held for years. If my body tells me it wants a big spoon of peanut butter, I listen and go get that from the kitchen, knowing I’m probably needing protein or fats. If it tells me it wants a huge salad, I’ll make that. And just the same, if it tells me if it wants a cupcake, I’ll have that too.
Conversely, I’ve also learned what foods trigger symptoms for me. I can eat a little bit of dairy without any repercussions, but if I eat large amounts I hurt. Therefore, I choose when I’m really wanting cheese, to eat my most favorite kind, and really savor it. I also know that red meat causes me a lot of pain, so even if my friends are all getting burgers, I likely choose to get something different because I know how my body will react if I do eat it.
“Intuitive eating is eating from a place of self-care,” says Hansen, “At times, someone might elect to eat a food they know will activate mild symptoms because they are valuing the pleasure of community that food is bringing in the moment. [At other times], it means opting out of a food experience we know will cause severe symptoms.”
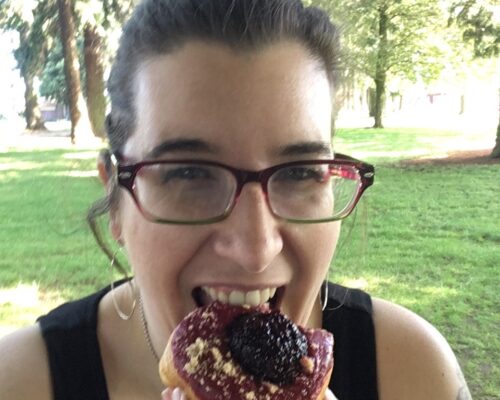
With intuitive eating I no longer feel like I’m restricting myself. I no longer feel shame or guilt while eating, or like I’ve somehow failed myself. Rather I now know I’m loving myself and my body through my food choices. I feel empowered and in control. As I reach for my fork — whether to pick up sweet potatoes or a slice of marionberry pie — I know I’m doing what is right for me in that moment, not what someone else has dictated for me.
Want to Get More Involved with Patient Advocacy?
The 50-State Network is the grassroots advocacy arm of CreakyJoints and the Global Healthy Living Foundation, comprised of patients with chronic illness who are trained as health care activists to proactively connect with local, state, and federal health policy stakeholders to share their perspective and influence change. If you want to effect change and make health care more affordable and accessible to patients with chronic illness, learn more here.