If there’s one thing we can agree about when it comes to the COVID-19 pandemic, it’s this: For many, the past year and a half has been an emotional rollercoaster. One day you feel afraid to leave the house and the next you’re anxious about pushback for wearing a mask in public. One day you feel angry that we’re still battling the pandemic going on two years, and the next you feel lonely and miss your pre-pandemic social life.
And all of this is even more magnified and extreme for people who are immunocompromised or high risk for coronavirus complications, including many people with inflammatory or autoimmune rheumatic conditions.
A new study, presented during ACR Convergence 2021, the annual meeting of the American College of Rheumatology, aimed to examine changes in physical, mental, and social health symptoms among rheumatic disease patients in the ArthritisPower research registry across a 15-month period during the COVID-19 pandemic. The researchers, who are from the Global Health Living Foundation (GHLF) and the University of Alabama at Birmingham, found that mental and social health worsened during certain periods.
“We wanted to learn more about how people in our community were doing physically, mentally, and socially and how this may have fluctuated throughout the pandemic,” says lead study author Kelly Gavigan, MPH, Manager of Research and Data Science at GHLF.
Capturing Patient-Reported Outcomes (PROs)
With chronic diseases like arthritis and related rheumatologic conditions, it is not always easy to get a holistic measure of health. Doctors can run blood tests to measure underlying inflammation or do imaging tests to identify joint swelling and damage, but this doesn’t fully capture the mental and social impact of having a disease. In other words, lab and imaging tests don’t provide a complete picture of how patients feel or how their condition is impacting their ability to function and lead a fulfilling life.
This is where patient-reported outcomes (PROs) play a vital role. They are typically short surveys that patients fill out about their symptoms and quality of life. PROs are also important during clinical trials to assess how different treatments or medications affect patients and their symptoms, from the patients’ point of view. For the study, researchers collected a total of 41,547 PROs via ArthritisPower, contributed by 2,226 patients. ArthritisPower is a patient-centered research registry from CreakyJoints and GHLF.
ArthritisPower uses PROs called PROMIS measures, which are developed by the National Institutes of Health. They are a publicly available system of highly reliable, standardized, and precise measures of patient-reported health outcomes used to measure health symptoms and health-related quality of life domains such as pain, fatigue, depression, and physical function, which are relevant across a variety of chronic conditions.
Participants were mostly white females (average age 52) with rheumatoid arthritis (RA). Other common conditions included osteoarthritis, fibromyalgia, and ankylosing spondylitis.
Participants took at least two ArthritisPower assessments at any time during the period from January 2020 through April 2021. The patient-reported outcome (PRO) surveys included the following domains and patient experiences.
Physical health
- Physical function
- Pain interference
- Fatigue
- Sleep disturbances
Mental health
- Anger
- Anxiety
- Depression
Social health
- Social isolation
- Emotional support
A Timeline of Emotional and Social Fluctuations
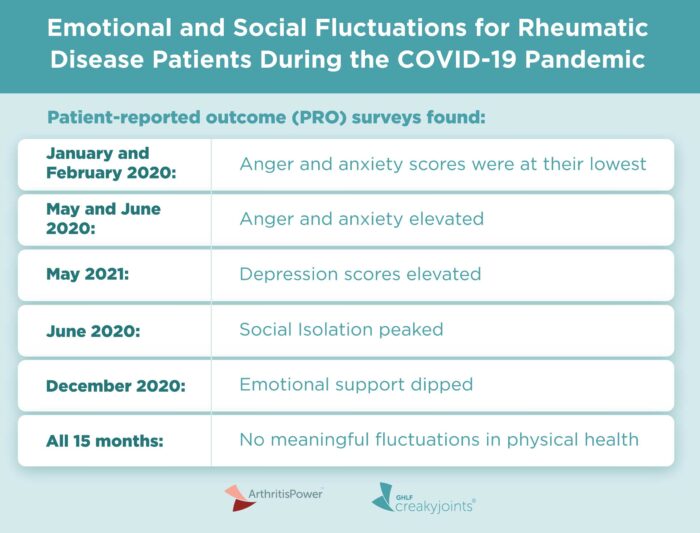
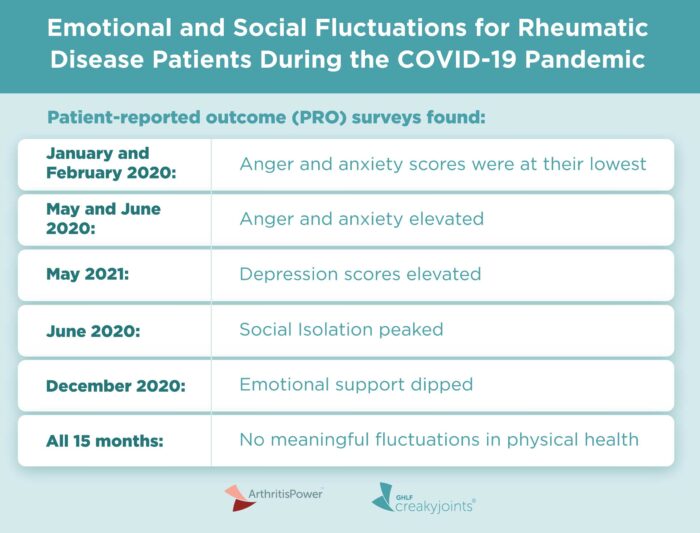
Though scores for self-reported physical health remained relatively stable throughout the COVID-19 pandemic period, scores for mental health fluctuated notably, particularly during the first U.S. wave between the months of April, May, and June 2020. Worsened emotional support also seemed to correspond with the winter holidays when people typically gather with family/friends, notes Gavigan.
Here is a summary of the findings:
- Anger and anxiety scores were lowest in January and February 2020, prior to U.S. lockdowns.
- During May and June 2020, anger and anxiety spiked when it was clear that the lockdown might continue indefinitely, and no vaccine was yet available.
- Depression scores, while also lowest in January 2020, increased significantly in May 2021.
- Social isolation peaked in June 2020.
- Emotional support was worst in December 2020, perhaps due to the spike in cases after the Thanksgiving holiday.
“While it’s not a surprise, it’s striking that mental health took a hit in May and June, and social isolation increased into the winter months of 2020 and 2021,” says Gavigan.
Perhaps unexpectedly, the PROs showed no meaningful fluctuations in physical health throughout the 15-month study period.
What These Findings Mean for You
These findings drive home the importance of tracking your mental and social health — not just your physical symptoms. Paying attention to your emotional well-being as well as your level of social support can help you better manage your overall health.
“It can be very powerful and helpful to be aware of your emotional health, which of course keeps changing when you have a chronic condition that you live with every day,” says study coauthor Shilpa Venkatachalam, PhD, Associate Director, Patient Centered Research, at CJ and GHLF and CoPrincipal Investigator of the ArthritisPower Patient-Powered Research Registry. “This is why it is important to track it. Those of us who live with chronic pain know well that anger, sadness, anxiety, feelings of helplessness, and frustration but also positivity, hope, and optimism can affect how we manage our overall health. This is important not just for us, as people living these conditions to know, but also for our doctors and loved ones to understand.”
The researchers hope these finding also urge providers and caregivers to be aware of and ask about the mental health concerns of people living with rheumatic disease.
Found This Study Interesting? Here’s How You Can Be Part of Arthritis Research
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
Gavigan K, et al. Changes in Patient-Reported Outcome (PRO) Scores During the COVID-19 Pandemic: Data from the ArthritisPower Research Registry [abstract]. Arthritis & Rheumatology. November 2021. https://acrabstracts.org/abstract/changes-in-patient-reported-outcome-pro-scores-during-the-covid-19-pandemic-data-from-the-arthritispower-research-registry/.
Interview with Kelly Gavigan, MPH, Manager of Research and Data Science at the Global Health Living Foundation.





