Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
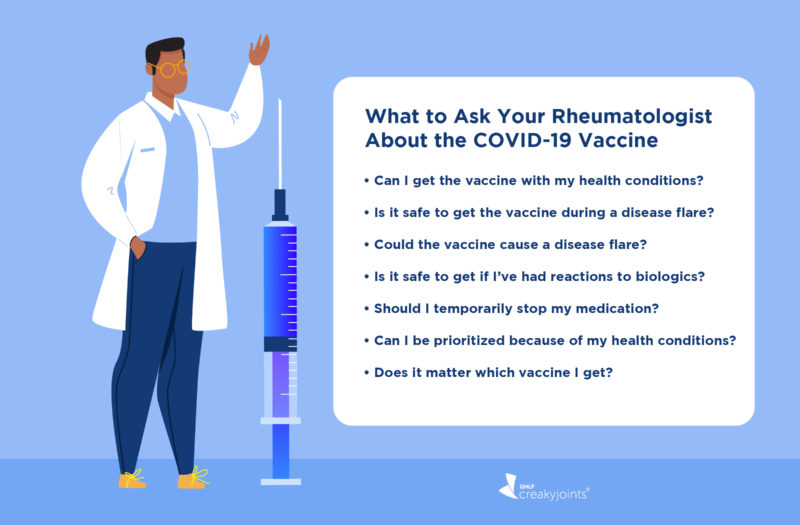
It’s understandable if have a lot of questions about the COVID-19 vaccine, especially if you live with an autoimmune or inflammatory disease like rheumatic disease. A new vaccine comes with many new questions for anyone — but on top of it, you may be concerned about disease flares, immunosuppressant medications, or potential reactions to the vaccine.
The reassuring news is that you can most likely get the COVID-19 vaccine, regardless of any of these factors. But if you’re nervous about getting the COVID-19 vaccine, here are seven questions to ask your doctor, and the advice they may give you based on new guidance from the American College of Rheumatology (ACR).
1. Should I get a COVID-19 vaccine even though I have rheumatoid arthritis or another autoimmune or inflammatory condition?
Beyond known allergies to vaccine components, the ACR guidance states that there are no known additional contraindications to COVID-19 vaccine vaccination for patients with autoimmune inflammatory rheumatic diseases (AIIRD).
In fact, it may be particularly important for you to get the COVID-19 vaccine if you have an underlying condition that could increase your risk of COVID-19 complications.
“The ACR’s COVID-19 vaccine guidance recommends all rheumatology patients with autoimmune and musculoskeletal conditions consider vaccination,” says David Karp, MD, President of the American College of Rheumatology. “Although there is limited data from large population-based studies, it appears that patients with autoimmune and inflammatory conditions are at a higher risk for developing hospitalized COVID-19 compared to the general population, and have worse outcomes associated with infection.”
In other words, it is a greater risk to your health not to get the vaccine, especially if you have an autoimmune or inflammatory condition.
For more information, check out our full guide on Getting a COVID-19 Vaccine: What to Know If You’re Immunocompromised.
2. I’ve been going through a disease flare. Is it still safe to get the vaccine?
The ACR guidance does not recommend delaying the COVID-19 vaccine based on disease activity and severity.
There may be some unique cases in which your doctor recommends waiting if you’re experiencing a severe flare (typically involving hospitalization) or temporarily on high levels of IV steroids (which may blunt your body’s immune system’s response to the vaccine). But in general, you should get the vaccine as soon as it becomes available to you, regardless of disease activity.
“In an ideal world, a patient would have low disease activity, but we don’t know how long it would take to reach that, and leaving a patient unvaccinated would pose a greater risk,” says Dr. Karp.
It is also difficult to forecast what your disease activity will be like in the coming weeks or months. While you wait for improvement that may or may not occur, you’ll still be at risk for contracting COVID-19.
“What you’re doing is saying: ‘Someday in the future, my rheumatic disease activity will be under better control and the vaccine might work better,’” says rheumatologist Jeffrey Curtis, MD, MPH, Professor of Medicine at the University of Alabama at Birmingham, who led the task force that created the ACR guidance. “However, you could be waiting for a really long time.”
The bottom line: In most cases, it’s better to get the vaccine as soon as it becomes available to you, rather than waiting for an uncertain amount of time for your disease activity to improve.
3. Could the vaccine cause my disease to flare?
Theoretically, it could, but that doesn’t mean it’s likely to happen, or that this type of response would be unique to the COVID-19 vaccine.
“There is a theoretical chance that any vaccine, not just the ones for COVID-19, could cause a disease flare,” says Dr. Karp. “However, it doesn’t appear to be very common with most vaccines.”
There isn’t data yet that shows flares of underlying rheumatic conditions are occurring specifically from the COVID-19 vaccine, but researchers are presently studying this. Many patients with rheumatic disease have already received the COVID-19 vaccine, and there are no clear indications that it has led to flare issues.
“I think it’s rather unlikely that the vaccine itself will flare up underlying rheumatic diseases,” says Stuart D. Kaplan, MD, Chief of Rheumatology at Mount Sinai South Nassau in Oceanside, New York.
However, the vaccine may have side effects that resemble some characteristics of a disease flare.
“What is more common [than the vaccine causing disease flares] is ‘reactogenicity,’ where a person has some physical symptoms because of their body generating an immune response,” adds Dr. Karp. “For example, someone might have fatigue, malaise, and/or low-grade fever after vaccination, and this shouldn’t necessarily be considered indicative of a flare. It may just be their immune system doing what it’s supposed to do.”
It can be easy to confuse vaccine side effects with classic symptoms of a rheumatic disease flare. In this case, it’ll be important to track your vaccine side effects carefully. Keep in mind that common vaccine side effects typically only last a few days, and include symptoms such as these, per the U.S. Centers for Disease Control and Prevention:
- Pain on the arm where you got the shot
- Swelling on the arm where you go the shot
- Fever
- Chills
- Tiredness
- Headache
All of this said, even if the vaccine were to cause a disease flare, it’s more important to be protected against COVID-19.
“The benefit of the COVID-19 vaccination outweighs the potential risk for any theoretical flaring of underlying disease, because we are dealing with a potentially lethal viral infection,” says Dr. Kaplan.
Beyond the risks of being infected with the virus, which can be life-threatening, researchers are finding that COVID-19 may cause the development of autoantibodies linked to autoimmune disease and could be tied to long-hauler symptoms associated with coronavirus. These autoantibodies mistakenly attack your own tissues or organs.
“We have to think about new-onset autoimmunity or disease worsening that happens after getting COVID-19,” says Dr. Curtis. “There are long-term autoimmune manifestations of just getting the infection that have nothing to do with the vaccine.”
For more information, check out our guide: Should You Get the COVID-19 Vaccine During a Disease Flare-Up?
4. Is it still safe to get the vaccine if I’ve had reactions to a biologic infusion/injection?
You’ll need to get your doctor’s approval, but you should be able to get the COVID-19 vaccine even if you’ve had reactions to a biologic infusion/injection. That’s because the CDC considers only two things to be a contraindication to the COVID-19 vaccine:
- Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a component of the COVID-19 vaccine (such as PEG or polysorbate)
- Immediate allergic reaction of any severity to a previous dose or known (diagnosed) allergy to a component of the vaccine
To see if you’ve had an allergic reaction to a component of the vaccines, here is a full list of the ingredients included in all three COVID-19 vaccines authorized in the United States.
The CDC states that it “considers a history of an immediate allergic reaction to any other vaccine or injectable therapy (i.e., intramuscular, intravenous, or subcutaneous vaccines or therapies [excluding subcutaneous immunotherapy for allergies, i.e., “allergy shots”]) as a precaution but not a contraindication to vaccination.”
“Reactions to biologic medications usually are specific for that drug,” says Dr. Karp. “Although we have no data on this particular situation, it should be safe for people to get the vaccine, as it is not similar to the biologic medication.”
For more information, check out our guide: Should You Get the COVID-19 Vaccine If You Have a History of Allergic Reactions to Infused or Injectable Medications?
5. Should I stop taking my immunosuppressant medication after getting the vaccine?
Your doctor will make this decision with you based on your current medication and disease activity. “We want to keep their disease under control, so patients should not skip their regular medication unless specifically recommended to do so,” says Dr. Kaplan.
The ACR guidance states that you should keep taking the following medications as prescribed:
- Hydroxychloroquine (Plaquenil)
- IVIG
- Low-dose glucocorticoids (ex: prednisone, daily dose < 20 mg)
- Sulfasalazine (Azulfidine)
- Leflunomide (Arava)
- Mycophenolate (CellCept)
- Azathioprine (Imuran)
- Cyclophosphamide (Cytoxan) (oral)
- TNF biologics (ex: Cimzia, Enbrel, Humira, Remicade, Simponi and Simponi Aria)
- IL-6 biologics (ex: Actemra, Kevzara)
- IL-1 biologics (ex: Kineret, Ilaris)
- IL-17 biologics (ex: Cosentyx, Taltz)
- IL-23 biologics (ex: Skyrizi, Tremfya)
- IL-12/23 biologics (ex: Stelara)
- Belimumab (Benlysta)
- Oral calcineurin inhibitors (ex: cyclosporine or tacrolimus)
The guidance states that it may be helpful to temporarily skip doses of a few certain medications before or after receiving the COVID-19 vaccine OR trying to time when you get the vaccine so it occurs at a certain point during the course of your treatment. But this should of course only be done under the guidance of your doctor and will depend on your disease status.
These medications include:
- Methotrexate
- JAK inhibitors (ex: Xeljanz, Olumiant, Rinvoq)
- Abatacept (Orencia), injectable or IV form
- Rituximab (Rituxan)
- Cyclophosphamide infusion
Read more here about the specific medication timing recommendations in the ACR guidance.
Even if your doctor decides you should not taper off any of these medications, it’s still worth it to get the vaccine.
“Even somewhat diminished protection is better than none,” says Dr. Karp. “If the vaccine is 90 to 95 percent protective for the general population, and somewhat less effective in patients on immunosuppressants, we feel that protection with the vaccine is better than if someone is not vaccinated.”
6. Can I be prioritized to get the vaccine because of my rheumatic condition?
It will come down to the guidelines your state sets for vaccine prioritization.
Each state will consider the CDC recommendations, which currently only cover the first few phases of vaccination and include groups such as:
- Health care personnel (Phase 1a)
- Long-term care facility residents (Phase 1a)
- Frontline essential workers (i.e., firefighters, police officers, etc.) (Phase 1b)
- People aged 75 years and older (Phase 1b)
- People aged 65 to 74 years (Phase 1c)
- People aged 16 to 64 with underlying medical conditions that increase the risk of serious, life-threatening complications from COVID-19 (i.e. cancer, chronic kidney disease, COPD, heart conditions, etc.) (Phase 1c)
- Other essential workers (i.e., those who work in transportation, food service, etc.) (Phase 1c)
The ACR guidelines make a push for those with rheumatic disease to be prioritized for vaccination before the non-prioritized general population of similar age and sex.
“It will vary by state, but based on our vaccine clinical guidance, we feel rheumatic disease patients should be included in prioritized groups,” says Dr. Karp. “The ACR is engaging with state leaders, urging them to prioritize patients on immunosuppressants in accordance with our recommendations and advocating that this prioritization be included in the next phases of their vaccine rollouts.”
7. Does it matter which vaccine I get?
Right now, the most important factor is that you get vaccinated — not which vaccine you get, experts say.
“Most people won’t have a choice,” says Dr. Curtis. “Maybe someday they will, but I think ‘Get the one you have access to’ is probably the main message.”
The Johnson & Johnson (J&J) COVID-19 vaccine was recently issued emergency use authorization by the U.S. Food and Drug Administration. It requires only one dose and doesn’t need to be stored at very cold temperatures, which will make its distribution much easier than the mRNA Pfizer and Moderna vaccines.
In a clinical trial of 44,000 people aged 18 and older, the J&J vaccine was found to reduce moderate to severe cases of COVID-19 by 66 percent 28 days after vaccination. In comparison, the Moderna and Pfizer vaccines are about 95 percent effective. But the three vaccines were equally effective at preventing very severe disease and serious complications, which is what’s most important.
That said, comparing the vaccines is a bit like comparing apples to oranges, because they weren’t head-to-head studies. They were conducted in different calendar timeframes, in different geographical locations, and while different virus variants were circulating — and even the definitions of symptomatic infection varied slightly, says Dr. Curtis.
“There are differences in methodologies and study design, and all of those things make it rather difficult to say with certainty that there’s truly a difference between the vaccines,” he says. “Get the one you immediately have access to. If and when the day comes that people actually have a choice, the answer might ultimately be different, but I don’t think that day is here and now.”
In terms of whether or not you would need to treat your medications any differently based on which vaccine you get, experts don’t expect the guidance to shift dramatically in light of the J&J vaccine authorization.
“I think the recommendations are mostly going to be the same,” says Dr. Kaplan. “As you see in the ACR guidelines, there are only a few medications which do need to be modified — for example, methotrexate is supposed to be held for one week after each vaccine dose. I think that would apply to the Johnson & Johnson vaccine as well.”
It’s expected that the ACR guidance for medications will be updated soon if any changes are needed for the Johnson & Johnson vaccine, says Dr. Curtis.
Get Free Coronavirus Support for Chronic Illness Patients
Join the Global Healthy Living Foundation’s free COVID-19 Support Program for chronic illness patients and their families. We will be providing updated information, community support, and other resources tailored specifically to your health and safety. Join now.
CDC’s COVID-19 Vaccine Rollout Recommendations. COVID-19. U.S. Centers for Disease Control and Prevention. February 19, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations.html.
COVID-19 Vaccine Clinical Guidance Summary for Patients with Rheumatic and Musculoskeletal Diseases. American College of Rheumatology. February 8, 2021. https://www.rheumatology.org/Portals/0/Files/COVID-19-Vaccine-Clinical-Guidance-Rheumatic-Diseases-Summary.pdf.
Interim Clinical Considerations for Use of COVID-19 Vaccines Currently Authorized in the United States. Vaccines & Immunizations. U.S. Centers for Disease Control and Prevention. March 3, 2021. https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html.
Interview with David Karp, MD, President of the American College of Rheumatology
Interview with Jeffrey Curtis, MD, MPH, Professor of Medicine at the University of Alabama at Birmingham
Interview with Stuart D. Kaplan, MD, Chief of Rheumatology at Mount Sinai South Nassau in Oceanside, New York
People with Certain Medical Conditions. COVID-19. U.S. Centers for Disease Control and Prevention. February 22, 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.