According to oft-stated health advice, one drink of alcohol a day is generally safe for women daily and two drinks a day is generally safe for men. But if you’ve been diagnosed for gout or are at risk for developing gout, you may need to cut back on drinking alcohol.
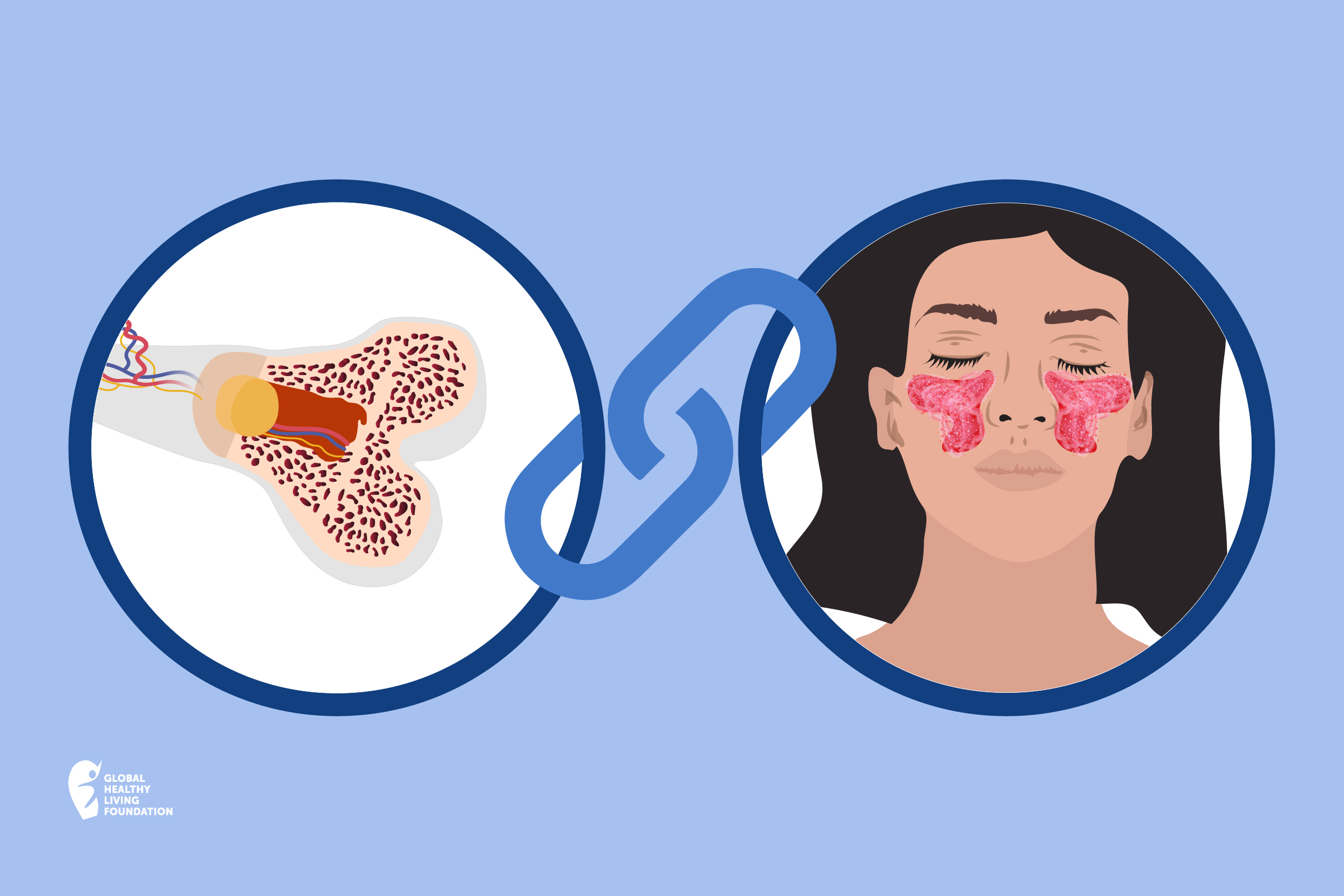
Gout is a type of arthritis where high blood levels of uric acid, a metabolism byproduct, start to crystallize in the joints, causing pain and swelling that is often sudden and severe. Gout typically develops in stages; in the first stage, uric acid levels are rising but not causing symptoms (called hyperuricemia); in the second stage, a person has started to experience painful gout attacks, called flares. As gout progresses, it becomes chronic, affecting more joints, with time between flares shortening.
Uric acid crystals can also form in the kidneys and cause kidney stones and can build up in various places in the body, such as below the skin and cause “bumps” called tophi. People with gout are also at risk for serious comorbidities, including heart disease and diabetes.
If you’re at risk for gout or have been diagnosed with gout, your doctor may advise you to cut back on certain foods that can contribute to gout symptoms, such as those high in purines, which break down into uric acid during digestion. On that list is also alcoholic beverages, including wine, beer, and spirits.
So is eliminating or avoiding alcohol a must when you have gout? You should talk to your physician for their recommendations about alcohol consumption and your specific health conditions, health history, and use with medications you take.
Here, learn more the connection between drinking alcohol and gout, and considerations to keep in mind for optimal health.
How Alcohol Affects Gout
Drinking alcohol affects gout risk in two main ways:
- Some alcohol (particularly beer) is high in purines, which are then broken down into uric acid.
- All alcohol — including beer, wine, and hard spirits — affect processes in the kidneys that in turn impact how uric acid is eliminated in urine.
“Alcohol makes the uric acid be pulled back into the body, with less [expelled] in the urine. This leads to elevated blood levels of uric acid,” says Theodore R. Fields, MD, a rheumatologist at the Hospital for Special Surgery in New York City. When uric acid isn’t excreted in urine, it further contributes to the formation of crystals in joints that cause intense pain and inflammation, says Jonathan Greer, MD, a rheumatologist with Arthritis & Rheumatology Associates of Palm Beach, Florida.
An analysis of multiple studies on alcohol consumption and gout — which included data on almost 43,000 people — found a “dose response of gout risk to alcohol consumption.” That means that the more alcohol people consumed, the greater the risk of developing gout.
Compared with people who never or rarely consumed alcohol, light drinkers (one drink or less a day) had a 16 percent increased risk of gout, moderate drinkers (more than one but less than three drinks a day) had a 58 percent increased risk of gout, and heavy drinkers (three or more drinks a day) had a 264 percent increased risk of gout.
Which Type of Alcohol Is the Worst for Gout?
All types of alcohol affect gout, but the impact on flares and symptoms may vary by type of alcohol, depending on which studies you look at. Some research suggests that beer is especially bad for gout because it contains higher levels of purines that break down directly into uric acid.
A 2004 study published in the medical journal The Lancet found that “alcohol is strongly associated with an increased risk of gout,” the study authors concluded. Risks varied according to type of alcoholic beverage:
- Two or more beers daily increased gout risk over non-beer drinkers two-fold
- Two shots of spirits daily increased gout risk over non-drinkers by 1.6 times
- Two four-ounce glasses of wine daily was not associated with a higher risk of gout
However, other research has found a link between wine consumption and gout risk. A study published in the American Journal of Medicine in 2014 looked at how much alcohol consumed over a 24-hour period was associated with a recurring gout attack. It found that all types of alcoholic beverages, including wine, were associated with an increased risk for recurrent gout attacks. Even though one drink didn’t raise the subjects’ risk for a gout attack by that much, having one to two drinks in a 24-hour period was associated with a 36 percent higher risk of recurrent gout attack, compared with those who had consumed no alcohol in that time period.
“Of the three types of alcohol, wine seems to be the least offensive, but it can still cause a problem,” says Dr. Greer. However, if some people think that by switching from beer to hard liquor or wine, they can avoid future attacks, experts want to correct that misconception.
“I appreciate that there has been some controversy about the effect of wine on gout,” says Dr. Fields, but all types of alcohol appear to affect the risk of gout or gout flares. “Until we have more data, my opinion on this is shaped by the fact that we know that alcohol has an effect on the kidneys,” he says. It would seem logical that alcohol in any form can have that effect, which will increase urate level, Dr. Fields adds.
“Therefore, pending further data, I advise my gout patients that alcohol in any form may have an adverse effect on gout. As with any food or drink that affects uric acid levels, people with gout need to pay special attention to them when they are either not on medication to lower urate level or are in the early stages of such treatment. That is when they are most vulnerable to food and drink that raises the urate level,” Dr. Fields says.
Can Eliminating Alcohol Reverse Gout?
In a word, no. Eliminating or cutting back on alcohol alone likely won’t lower uric acid levels enough to effectively treat gout. For many people with gout, the target uric acid level is less than 6 mg/dL. “If a person with high levels of uric acid goes on a diet, loses weight, eliminates high-purine foods like shellfish and stops drinking beer, they can lower their uric acid from, say, 10 to 9, but usually not much lower. Dietary improvements are still not enough — the patient has to be on uric acid-lowering medication at this level,” says Dr. Fields.
It is a myth that gout is a dietary disease, and that watching your diet (limiting alcohol, red meat, shellfish, high-fructose corn syrup, and organ meats like liver) will be enough to manage gout.
“Gout is a genetic disease and extremely few people can make enough of a change in their blood uric acid level with diet to control their gout,” says Dr. Fields. That said, it’s still important for people to limit those foods and beverages mentioned as part of their treatment, especially in the first six months after they start uric acid-lowering therapy when the patient is vulnerable to flares since these foods and drinks can make gout worse. “Watching your diet, especially early in treatment, can make a difference,” says Dr. Fields.
How Much Alcohol Is Safe to Drink if You Have Gout?
People with gout should limit their intake of alcohol, especially in the first six months after starting a uric acid-lowering medication such as allopurinol to manage it, suggests Dr. Fields. “Once a person is on allopurinol and hasn’t had any gout flares for six months, often they can liberalize their alcohol intake, at least a little, and not get flares,” he says. This seems to be because the allopurinol has led to uric acid being pulled out the joints, so that there isn’t an “overflow” situation when the uric acid suddenly rises due to alcohol.
That aforementioned American Journal of Medicine study mentioned above found that when people were on allopurinol, it helped mitigate the effects of their alcohol intake. Taking colchicine, a medicine used to treat gout flares, also helped decrease the effects of alcohol, but to a lesser extent.
If you’ve been diagnosed with gout and are managing it with medication for the long term, occasional intake of high-purine foods, like red meat and shellfish, and a small amount of alcohol is generally okay, says Dr. Fields. “High quantities of any of these have a good chance of setting off gout flares, especially in the untreated patient or the patient early-on in the use of a medication such as allopurinol.”
Use Our ArthritisPower App to Manage Your Gout
Join CreakyJoints’ patient-centered research registry to track your symptoms, disease activity, and medications — and share with your doctor. Learn more and sign up here.
Keep Reading
Choi HK, et al. Alcohol intake and risk of incident gout in men: a prospective study. The Lancet. April 2004. doi: https://doi.org/10.1016/S0140-6736(04)16000-5.
Gibson T, et al. Beer drinking and its effect on uric acid. Rheumatology. August 1984. doi: http://dx.doi.org/10.1093/rheumatology/23.3.203.
Gout. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Gout.
Gout. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/gout/symptoms-causes/syc-20372897.
Interview with Theodore Fields, MD, rheumatologist at the Hospital for Special Surgery in New York City
Interview with Jonathan Greer, MD, a rheumatologist with Arthritis & Rheumatology Associates of Palm Beach, Florida
Is There a Correlation between Alcohol Consumption and Gout? Alcohol.org. https://www.alcohol.org/effects/gout.
Kaneko K, et al. Determination of purine contents of alcoholic beverages using high performance liquid chromatography. Biomedical Chromatography. August 2019. doi: https://doi.org/10.1002/bmc.1197.
Neogi T, et al. Alcohol quantity and type on risk of recurrent gout attacks: An internet-based case-crossover study. The American Journal of Medicine. April 2014. doi: http://dx.doi.org/10.1016/j.amjmed.2013.12.019.
Towiwat P, et al. The association of vitamin C, alcohol, coffee, tea, milk and yogurt with uric acid and gout. International Journal of Rheumatic Diseases. doi: https://doi.org/10.1111/1756-185X.12622.
Wang M, et al. A meta-analysis of alcohol consumption and the risk of gout. Clinical Rheumatology. November 2013. doi: http://dx.doi.org/10.1007/s10067-013-2319-y.