If you Google “lupus symptoms,” it can be easy to fall down a rabbit hole. After all, this condition is notoriously difficult to diagnose and may include many symptoms that overlap with other autoimmune diseases. Lupus signs and symptoms can range from fatigue and fever to weight loss and achy joints.
However, there are a few key clues that may point your doctor toward a lupus diagnosis. Being aware of these lupus indicators is important as you work with your provider to determine what’s causing your symptoms and advocate for a correct diagnosis.
Here’s what you need to know about lupus symptoms that may overlap with other conditions, plus the symptoms that can distinguish it from other diseases.
Lupus Symptoms That Are Similar to Other Autoimmune Diseases
First, let’s start with the symptoms that make lupus so difficult to diagnose — those that are present in several other diseases as well, including other autoimmune diseases.
“Constitutional symptoms [those that impact the entire body] can be present in many other autoimmune diseases, as they are symptoms from chronic inflammation caused by a systemic autoimmune disease,” says Kichul Ko, MD, rheumatologist and Associate Professor of Medicine at The University of Chicago Medicine.
Here are just a few examples of lupus symptoms that may overlap with other diseases:
- Joint involvement can resemble rheumatoid arthritis, since both lupus and rheumatoid arthritis may lead to symmetrical swelling, pain, and redness in the fingers and wrists.
- Dry eyes and mouth, which is a hallmark of the autoimmune disease Sjogren’s syndrome, can also occur in lupus patients.
- Kidney disease is a lupus comorbidity that can lead to decreased kidney function and increased protein spill in the urine. This can resemble systemic vasculitis, an autoimmune disease involving the inflammation of blood vessels.
- Some lupus skin rashes look identical to a rash from dermatomyositis, an inflammatory disease. Experts aren’t sure what causes dermatomyositis, so it’s not classified as an autoimmune disease, but it’s similar to lupus and other autoimmune conditions, per the Cleveland Clinic.
- Pleurisy, the inflammation of the lung lining, is a lupus symptom that can also occur in other autoimmune diseases like rheumatoid arthritis and Sjogren’s syndrome.
Symptoms That Distinguish Lupus from Other Autoimmune Diseases
One important lupus fact: There is no single indicator of this disease. Your doctor may look at your medical history, do a physical exam, and draw lab work if you present with new and unexplained symptoms such as joint pain, rashes, and fatigue that could be considered lupus symptoms.
You might be referred to see a rheumatologist if lab results show signs of anemia, low platelets, low white cell counts, a decline in kidney function, or abnormal autoimmune tests, which can all be present in lupus.
Your provider will also consider the specific combination of symptoms you’re experiencing.
“Lupus is less likely to cause erosions in the joints than rheumatoid arthritis, and the joint pain can present with less swelling than as seen in rheumatoid arthritis,” says Zeba Faroqui, MD, rheumatologist at PRINE Health and Founder and CEO of Dr. Zeba Consulting. “In contrast, lupus presents more commonly with skin rashes than rheumatoid arthritis does.”
If you have lupus, you may also have a wider variety of symptoms than if you were dealing with a condition like rheumatoid arthritis. In addition to, say, joint pain, you may also encounter the following:
- Change in urine
- Chest pain
- Fatigue
- Frequent bleeding or bruising
- Neuropathy-like symptoms (those involving the nerves, like pain or pins-and-needles feelings)
- Oral or nasal ulcers
- Shortness of breath
“The presentation of lupus symptoms is far more varied than other autoimmune diseases such as rheumatoid or psoriatic arthritis, which each typically present with their own classic pattern of joint pain, stiffness, and swelling,” says Dr. Faroqui.
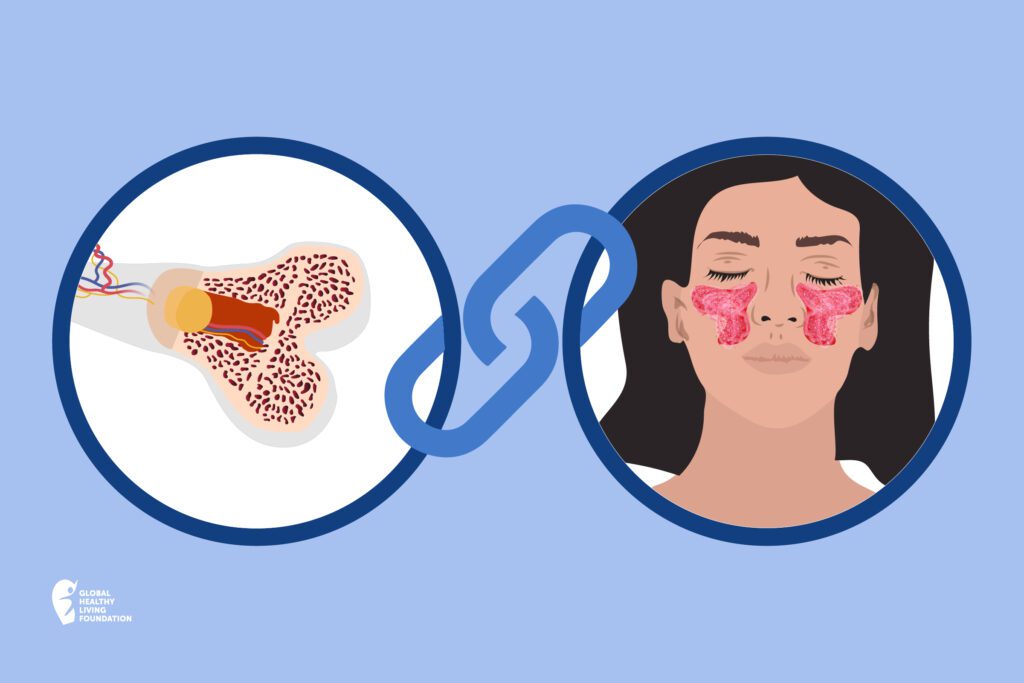
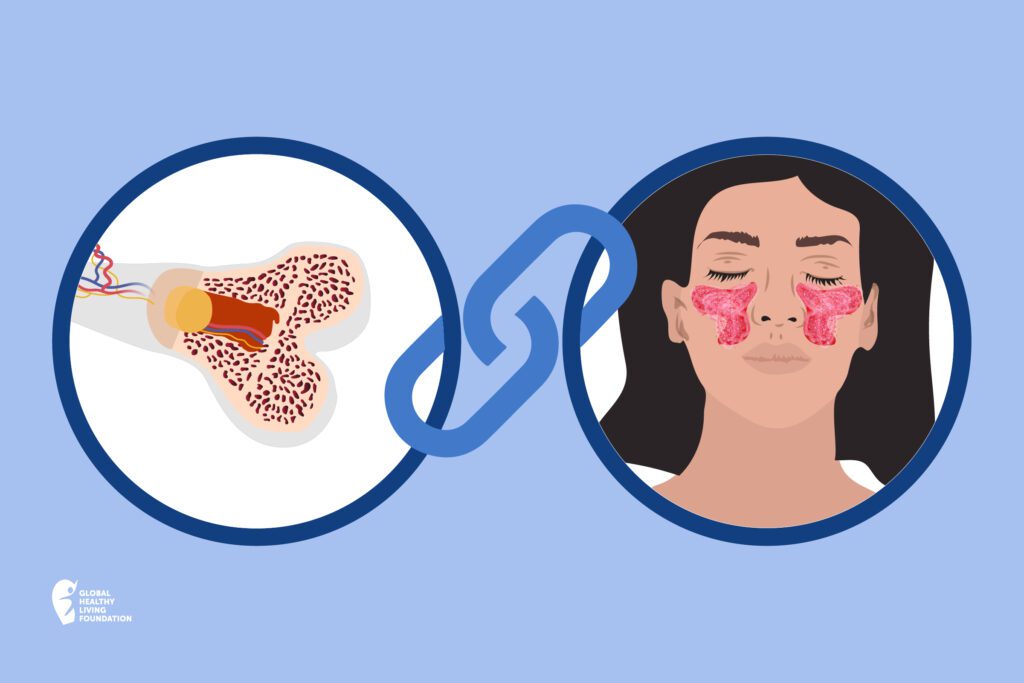
The most distinctive sign of lupus is a butterfly rash that resembles the wings of a butterfly and spans across the cheeks, per the Mayo Clinic. This rash can be raised or flat and is seen in about 46 to 65 percent of lupus patients, according to a 2019 article in QJM: An International Journal of Medicine.
However, this is not the only type of rash that may occur in lupus.
“The presentation of lupus rashes can vary dramatically, so it is best to consult with a rheumatologist or dermatologist for further evaluation,” says Dr. Faroqui. “Many rashes may present upon reaction to sunlight exposure, which is known as photosensitivity. In approximately 20 percent of lupus patients, skin rash is their first symptom.”
How Your Doctor Will Diagnose Lupus
There’s no blood test that’s fully diagnostic for lupus, but this type of lab work is still important as your doctor considers what might be causing your symptoms.
“ANA, or anti-nuclear antibodies, can be a helpful test,” says Dr. Ko. “If it comes back negative, then the chances are the patient does not have lupus, although negative ANA lupus can also occur on rare occasions.”
Positive testing for certain types of lab work like ANA tests, which many commonly think of as “the lupus test,” is high. Between 12 to 16 percent of the U.S. population may test positive for the ANA test, per a classic study in the journal Arthritis & Rheumatism.
“Many of these ANA tests are negative on repeat testing, or the patients do not have the clinical symptoms that would indicate lupus,” says Dr. Faroqui. “Rheumatologists must make the diagnosis taking the patient’s history and exam in mind.”
For instance, if you have positive autoimmune tests but do not have correlating symptoms, you might not necessarily have autoimmune disease like lupus. In that case, your doctor may believe your case warrants further testing or monitoring going forward.
After examining you, looking at your history, and reviewing your lab tests, your doctor will look at your whole picture of health to determine if your symptom pattern fits one diagnosis over others. Once they have an hypothesis, your provider will order additional tests to support their theory.
“Let’s say the patient has positive anti-dsDNA antibodies, which are more specific for lupus, and negative rheumatoid factors and anti-CCP antibodies, both of which are for rheumatoid arthritis,” says Dr. Ko. “Their X-rays do not show evidence of rheumatoid arthritis, which can cause chronic damage in the joints. In this case, the patient would more likely be diagnosed with lupus.”
One final piece of advice from experts: Make sure you’re working with a rheumatologist who has experience in this diagnostic process — and seek a second opinion when needed. “In order to diagnose lupus, it is important to see a rheumatologist who is trained in distinguishing between different autoimmune diseases,” says Dr. Faroqui.
Be a More Proactive Patient with PatientSpot
PatientSpot (formerly ArthritisPower) is a patient-led, patient-centered research registry for people living with chronic conditions. You can participate in voluntary research studies about your health conditions and use the app to track your symptoms, disease activity, and medications — and share with your doctor. Learn more and sign up here.
Interview with Kichul Ko, MD, rheumatologist and associate professor of medicine at The University of Chicago Medicine
Dermatomyositis. Cleveland Clinic. May 11, 2022. https://my.clevelandclinic.org/health/diseases/15701-dermatomyositis.
Interview with Zeba Faroqui, MD, rheumatologist at PRINE Health and Founder and CEO of Dr. Zeba Consulting
Lupus. Mayo Clinic. October 21, 2022. https://www.mayoclinic.org/diseases-conditions/lupus/symptoms-causes/syc-20365789.
Kumar RR, et al. Butterfly rash: hallmark of lupus. QJM: An International Journal of Medicine. April 26, 2019. https://doi.org/10.1093/qjmed/hcz091.
Satoh M, et al. Prevalence and Sociodemographic Correlates of Antinuclear Antibodies in the United States. July 2012. Arthritis and Rheumatism. https://doi.org/10.1002/art.34380.





