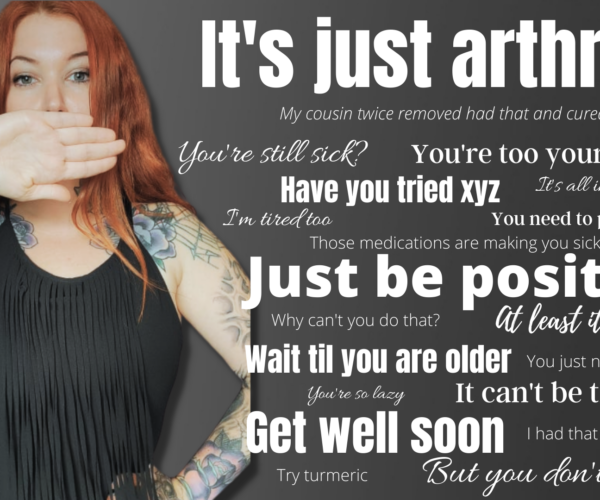
Arthritis comes with many stigmas and misconceptions, some which people don’t even realize they are bringing up when they talk to us about our diagnosis. While there is no perfect way to respond when someone tells you they have arthritis, there are some things you can definitely avoid saying. There are phrases that come off as rude or naive to what someone with arthritis is experiencing. Even those with the best intentions might say something disappointing or disheartening.
Here are some examples of what you should not say to somebody living with arthritis — and why you should avoid saying these phrases to anyone living with a chronic health condition.
A good rule of thumb: Think about how would you want those around you to respond if you were diagnosed with arthritis or another type of chronic illness. Understanding? Support? Validation? Listening without judgment, advice, or distraction? Those go a lot further than these comments below.
“But you don’t look sick.”
The curse of living with an invisible illness.
Unfortunately, we hear this all the time because arthritis is an invisible illness that can strike anyone at any age. The truth is you don’t need to look sick to be sick. There are many other types of invisible illnesses out there: multiple sclerosis, diabetes, epilepsy, even cancer can be invisible. Just because it is invisible, it doesn’t mean that someone is not living with it or that it’s not severe.
We never know what someone is going through inside, so we should always remind ourselves that even if someone doesn’t look ill, they may need that disability parking spot or seat on the bus.
“It’s only arthritis.” “It can’t be that bad.” “You’ll be fine.”
Unless you are living with the pain of arthritis, you shouldn’t judge the pain of arthritis. It absolutely can be that bad when living with arthritis. Minimizing our condition with comments like “it can’t be that bad” or “you’ll be fine” is infuriating when in reality we are feeling anything but fine.
There has long been the misconception that arthritis is not a serious condition, with osteoarthritis being the only form, however that isn’t the truth. There’s over two hundred forms of arthritis, many of which are very serious conditions. There is no cure for arthritis and it has a massive impact on someone’s daily life. Arthritis is the main cause of long-term disability, often coming before heart disease, lung disease, and diabetes. Saying “it’s only arthritis” is like saying “you’re only going to be in pain and disabled for the rest of your life.” How is that ok?
“At least it’s not cancer.”
Cancer is not the only disease out there that we should be fearing and it shouldn’t be the only disease out there when it comes to compassion from others. Unfortunately, a lot of times when we tell people about our arthritis diagnosis we are met with “well at least it’s not cancer” like it’s the only serious illness that has an impact on someone’s life.
When I was diagnosed with rheumatoid arthritis at 29, I had family members brush off my diagnosis and boost how they were cancer survivors. Hearing this made me feel as if everything was in my head; like I was making it all up. It made me think I was weak.
Arthritis can have serious consequences on our lives. We are immunocompromised so have a harder time fighting off infections; we’re at more risk for certain different kinds of cancers; and we are often plagued with many comorbidities like heart disease.
“Imagine what it will be like when you are older.”
I’m not sure how this one is supposed to be supportive or comforting but telling somebody to imagine their lifetime of pain and disease because they have arthritis at a young age is a very depressing thing to hear.
Just don’t. There’s no need to point that out to us. We already know it.
“You are too young for that.”
Did you know more children are diagnosed each year with arthritis than cancer?
Anyone can have arthritis, even babies. Arthritis affects people of all ages, races, and sexes. It is the most common cause of long-term disability in North America and yet it still comes with a lack of understanding unless someone is living with the condition themselves or someone close to them lives with it. When I hear “I’m too young to have arthritis” from people in the medical field, I’m left seriously questioning their training.
“I know someone with that condition and they can….”
This comment can come in two forms: claims that they know someone who cured their condition or questioning why someone else they know with arthritis can do something I can’t — like work full time.
Just because you know somebody who claims to have cured their arthritis doesn’t mean I can do the same. The same goes with working; everyone’s arthritis is different.
My form of arthritis doesn’t have a cure. Most forms of arthritis have no cure. Arthritis can go into remission but there’s always the risk of coming out of remission or the medications used to get to remission becoming ineffective. Getting an arthritis diagnosis and finding the right treatment is a very lengthy process.
“Have you tried XYZ…”
Please, please, refrain from unsolicited advice. Instead, support us and ask us what we find helps us. Trust me, if we’ve been living with pain and fatigue for a long time, chances are we have tried or researched everything we can try. The sea of suggestions and advice can be very overwhelming and even harmful if autoimmune diseases or arthritis are not properly understood.
“Get well soon.”
I know they mean well; really they do. “Get well soon” is something that people automatically say when you tell them you’re dealing with an illness. However, arthritis has no cure so telling us to get well soon isn’t possible for everyone. Why not instead acknowledge that we fight every single day and that you support us?
“Just push through it.”
The only one to decide when we need to push through the pain in the fatigue of arthritis is ourselves. Don’t tell anybody to just push through their condition when you don’t know what it’s like to live with it. When we do push through it we pay for it later. It takes time and trial and error to figure out where we can draw the line between pushing too hard and pacing ourselves just right.
“Can you just take something for that?”
Over-the-counter pain medications don’t even come close to touching the pain of arthritis, so we can’t really just take something. Treating arthritis is unfortunately a lot more complicated than that and involves a number of complex medications and treatments. Finding something that controls our disease can take months or even years.
“You should exercise more.”
Unless you are our physiotherapist or doctor, then you can zip it. We all know exercise is good for us, we hear this a lot and everywhere we turn for advice says “you need to exercise.” However, there are times when arthritis makes exercise extremely difficult. With uncontrolled disease, like at the beginning of someone’s diagnosis, exercise is likely the last thing on their mind. You also need proper knowledge on how to exercise safely with arthritis.
“Maybe you should lose weight or change your diet.”
Feeling better with arthritis goes beyond weight loss and eating healthy. While lowering your weight if you are overweight will help release load off your joints and improve your health, it still won’t cure arthritis. Nor will any amount of healthy eating and exercise. Weight fluctuates for many people with arthritis. Some of our drugs cause weight gain or we may gain weight when we go through a flare and can’t exercise, or when our depression is raging. Why make us feel worse with hurtful comments about our weight?
“You just have to be positive.”
Being forced to be positive all the time is more toxic to us than beneficial. Yes, having a positive mindset helps a lot but so does releasing our negative emotions and concerns. No amount of positive thinking will change the fact I have a serious debilitating illness that has negative impacts on my everyday life. Depression and anxiety are common among those with arthritis, which can make positive thinking seem like an impossible feat.
“I wish I didn’t have to work — you are so lucky to stay home all day.”
Being able to take time off of work to focus on my health was great at the beginning, my body really needed the rest. After nearly a decade of not being able to work, it’s actually not all that it’s cracked out to be. Disability doesn’t cover many luxuries like trips or expensive entertainment. It gets boring fast — and, on top of that, I’m dealing with chronic illness at home. Some days I feel trapped inside my home because of arthritis.
“But you could yesterday.” “Stop using arthritis as an excuse.”
One of the trickiest parts to understanding this disease is that one day we can have a great day where we can accomplish a lot and the next day we can be bedridden unable to care for ourselves in just simple basic ways a healthy person doesn’t think twice about. We don’t always know exactly when those days will be, however they can be promised usually after a stressful or physically exhausting event. They can pop out of nowhere at any time and they don’t care what plans we have scheduled.
Think we are a flake? Truth is chronic illness is unpredictable and bumpy. It’s the disease that’s flakey; not me.
16. “I’m tired too.”
We all get tired, that is guaranteed every night before we go to bed or if we don’t get enough sleep. Tiredness and fatigue are not the same thing. The kind of tiredness that I’m experiencing is an autoimmune disease, so that means my immune system is attacking the body’s own healthy tissue and causing symptoms of a disease, fatigue. No matter how much rest I get or how healthy I eat, or how much coffee I drink, I will always be at an extreme level of tired because that’s what fatigue is.
17. “You’re so lazy.”
Imagine being trapped with a mind that wants to do a lot but a body that wants to do the opposite? Or feeling so foggy, overwhelmed, in pain, or weighed down with unrelenting tiredness that won’t go away — that’s arthritis and it’s not about being lazy. Calling us lazy is hurtful and not supportive at all.
Be a More Proactive Patient with ArthritisPower
Join CreakyJoints’ patient-centered research registry to track your symptoms, disease activity, and medications — and share with your doctor. Sign up.