Margaret Liang Harris was convinced that the pain in her joints was rheumatoid arthritis (RA). About six months after she had her first child, she got an ache in her elbow that was unlike anything she had experienced before; it felt like it was coming from deep inside her joint. And it was just as her own mother — who had been diagnosed with RA years back — had described her own pain.
“I went to my primary care doctor and told him my suspicions, but he didn’t believe me because I didn’t present with the ‘right’ signs,” she says. He drew her blood and tested it for everything else under the sun: blood sugar, cholesterol, liver and kidney function, and on and on — all of which came back normal. Liang Harris insisted that her blood be tested for rheumatoid arthritis, and eventually she got her RA diagnosis.
“My doctor was surprised,” she recalls. “I was not.”
Here’s the thing with rheumatoid arthritis: In early stages, it can be difficult to diagnose in some patients. Part of the reason is that RA can’t always be confirmed with just one test. And the more distinctive or obvious signs — such as deterioration or deformity in a joint — occur later once RA has progressed, explains Vinicius Domingues, MD, assistant professor of medicine at Florida State University and CreakyJoints medical advisor.
Rheumatoid arthritis is a type of inflammatory, autoimmune arthritis that typically causes joint pain, swelling, and stiffness in symmetrical joints throughout the body. Rheumatoid arthritis occurs when the immune system attacks the lining surrounding a joint,called the synovium. However, in some people RA can present less typically, which can make getting the right diagnosis tricky.
Rheumatoid Arthritis Blood Tests: Clearing Up Confusion
You may have heard about blood tests for certain antibodies helping to clinch a diagnosis of RA. But some blood tests used to help diagnose RA can be negative. Most people with RA are what’s known as seropositive — they have abnormally high levels of rheumatoid factor (RF) or anti-citrullinated peptides (anti-CPP) antibodies in their blood. These antibodies are produced by the immune system and play a role in the immune system attacking healthy joints and tissue.
But research shows up to half of people with RA are seronegative, which means they don’t have either of these antibodies in their blood.
“These patients may still have classic RA symptoms, such as joint pain and morning stiffness,” says Dr. Domingues. “But because this basic screen is negative, physicians may not refer the patient to a rheumatologist and instead start them on another treatment plan, when they should be taking RA medications.”
The Importance of Seeing a Rheumatologist
That’s why it’s important to see a rheumatologist if you think you might have arthritis symptoms, advises Elaine Husni, MD, MPH, vice chair of the department of rheumatic and immunologic diseases and director of the Arthritis Center at the Cleveland Clinic. A rheumatologist is a doctor who specializes in treating arthritis and certain autoimmune disease. They are trained to diagnose RA at an earlier stage, which may minimize unnecessary testing and treatment and help to improve overall patient outcomes.
That advice would have benefited CreakyJoints member Lindsey Stambaugh. Her symptoms also began after the birth of her son. Her first doctor told her the pain was psychological; a few years later, she was sent to a pain clinic, where she was given medications and injections to mute the symptoms. It wasn’t until Stambaugh started working in a rheumatologist’s office, who recognized symptoms during one of her flare-ups, that she was evaluated for and diagnosed with RA.
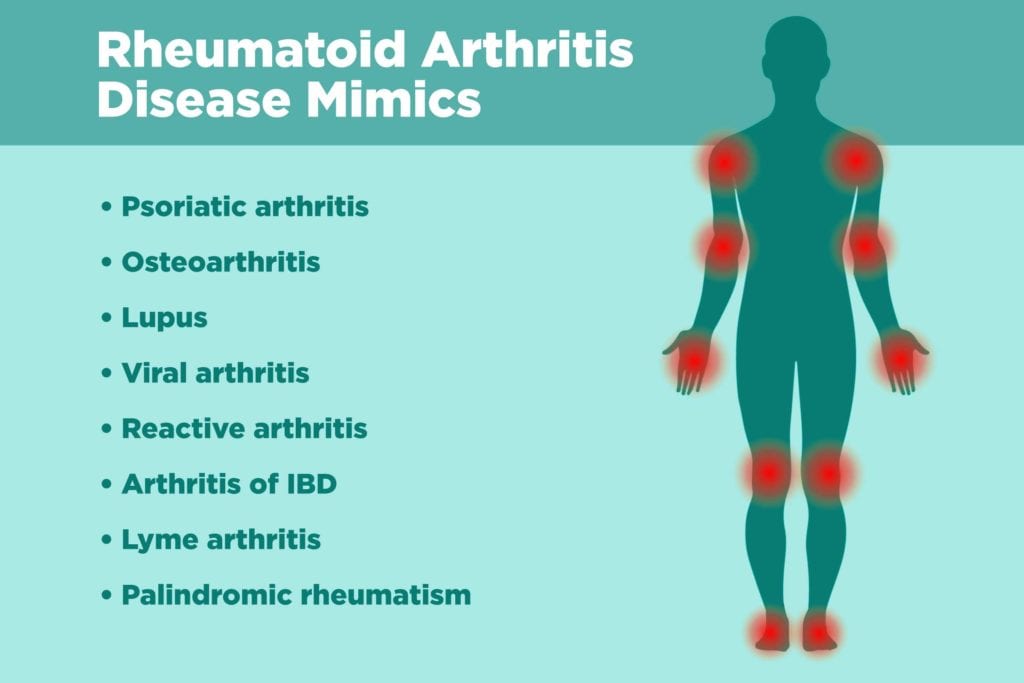
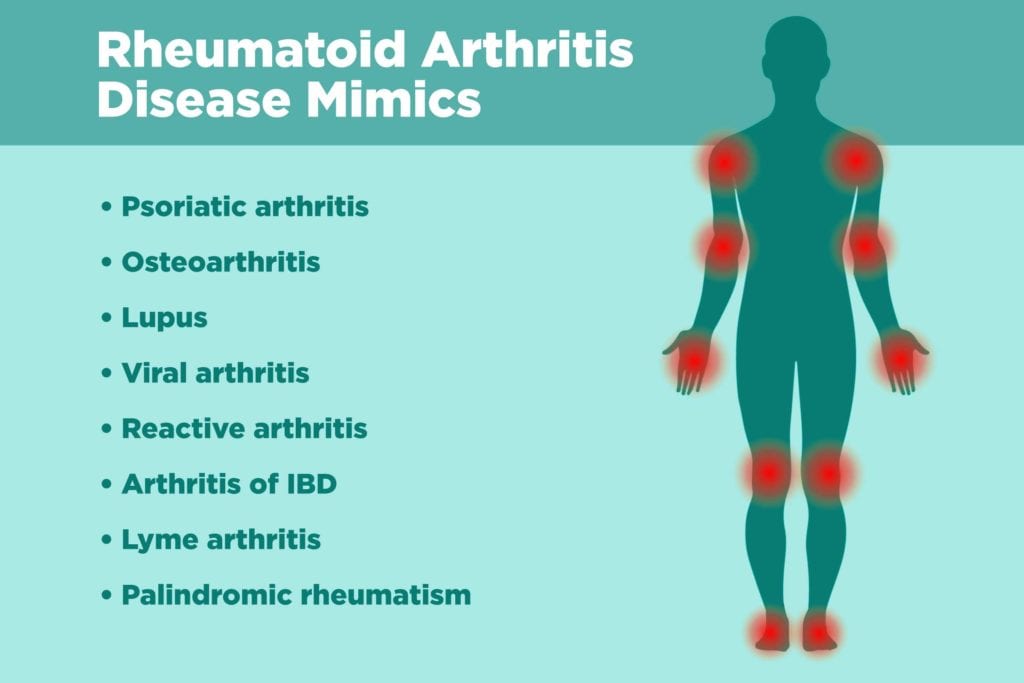
Conditions that Can Mimic RA
Another reason RA may be tough to diagnose in early stages is that some initial signs and symptoms can be difficult to distinguish from other conditions. Viral infections, other kinds of arthritis, and other autoimmune diseases may all be mistaken for RA, depending on which specific constellation of symptoms you have. It’s important to learn about these different diseases so you can be sure to be as specific as possible when describing your medical history to your doctor.
Some of the conditions that mimic rheumatoid arthritis include:
Psoriatic Arthritis
This form of inflammatory arthritis can be tough to distinguish from RA, particularly if there are no obvious symptoms of psoriasis, a different autoimmune disease that causes red patches of skin topped with silvery scales. Like RA, psoriatic arthritis can cause painful, swollen joints that are warm to the touch. However, psoriatic arthritis is more likely to also cause sausage-like swelling in the fingers and toes (called dactylitis), nail changes, foot pain (especially at the back of your heel or along the sole of your foot) which can signal enthesitis (or inflammation of soft tissue where it meets the bone), and lower back pain. Read more about psoriatic arthritis symptoms here.
Osteoarthritis
The main difference between OA and RA: RA is a systemic inflammatory condition; osteoarthritis (OA) is primarily a degenerative disorder where the cartilage that cushions the joints breaks down over time. OA is more likely to be confused with RA in a middle-aged or older patient when it involves small joints of the hands.
But some symptoms of OA and RA will differ. Swelling, for example, is hard and bony in OA and soft and warm in RA. Stiffness occurs in both conditions, but in RA, it’s worse in the morning or after resting the joint. In OA, a joint may get stiff after effort or overuse. (However, there is a form of OA called erosive or inflammatory OA, which affects joints in the hand and may also be confused for RA.) Blood tests and imaging studies can also help differentiate the two conditions.
Lupus
When lupus, a systemic autoimmune disease, affects the joints, it can cause symptoms similar to RA. Most people with lupus also experience flares, where symptoms get worse, then improve or disappear. Other similar signs of lupus and RA include fatigue, fever, and dry eyes. In some people with lupus, joint deformity may occur as well. The difference, however, is that it’s caused by loosening and lengthening of tendons and ligaments, not by joint erosion.
Some symptoms that are distinct to lupus include: a butterfly-shaped rash across the cheeks and nose, skin sensitivity to light, and Raynaud’s phenomenon, a condition where fingers and toes turn white or blue when exposed to cold or during stressful periods.
Viral Arthritis
Some viral infections — such as parvovirus B19 — can cause symptoms in multiple joints that may be mistaken for RA. In children, parvovirus may cause fever and rash on the cheeks, but usually not joint problems. Adults who’ve been in contact with children who have parvovirus, however, may develop joint soreness, typically in the hands, wrists, knees, and ankles. Joint symptoms from parvovirus usually clear up quickly, lasting only from a few days to several weeks.
Another virus that causes arthritis joint pain is called Chikungunya. It’s caused by bites from infected mosquitoes, is increasingly reported in travelers, and causes symptoms that closely mimic RA. Outbreaks have occurred in countries such as Italy, India, Indian Ocean islands, and those in the Caribbean. In some people, joint pain from Chikungunya can last for months. Doctors can use blood tests and exposure history to distinguish viral arthritis from RA.
Reactive Arthritis
Reactive arthritis is joint pain and swelling triggered by a bacterial infection in another part of your body — most often your intestines, genitals, or urinary tract. A number of bacteria can cause reactive arthritis; some are foodborne, such as salmonella and campylobacter, others are transmitted sexually, like chlamydia. Reactive arthritis usually targets your knees and the joints of your ankles and feet. The physical signs of both reactive arthritis and RA can be identical in the knees. Doctors usually diagnose reactive arthritis using history of infection, joint and muscle involvement, and imaging tests. Read more about reactive arthritis here.
Arthritis of IBD
People with inflammatory bowel disease (IBD) — including ulcerative colitis and Crohn’s disease — may develop peripheral arthritis that affects the knuckles and can be mistaken for RA. IBD-related arthritis can also cause symptoms in the elbows, wrists, knees, and ankles. Arthritis of IBD may be missed if symptoms of IBD — such as abdominal pain, diarrhea, or blood in the stool — aren’t prominent. Although no specific test can make a definitive diagnosis, X-rays and lab and blood tests can be used to rule out other causes of joint pain.
Lyme Disease
The most common tick-borne disease, Lyme disease can lead to bouts of severe joint pain and swelling, particularly in the knee. It can be confused with a number of conditions, including RA. That’s what happened to CreakyJoints member Rachel Drucker.
“I was misdiagnosed with Lyme’s disease by an infectious disease doctor, who prescribed me antibiotics,” she shared on Facebook. After three weeks on the meds with no pain relief, she sought the opinion of another doctor, who diagnosed her with RA.
Some signs that differentiate Lyme arthritis from rheumatoid arthritis: Pain can shift from one joint to another in Lyme disease, and Lyme arthritis rarely affects small joints in the hands and feet. Lyme is also often indicated by a rash in a bulls-eye pattern that expands slowly after several days. If you don’t have the characteristic rash, your medical history, a physical exam, and lab tests can help identify antibodies to the Lyme bacteria can help confirm or rule out the diagnosis.
Palindromic Rheumatism
Palindromic rheumatism is rare form of inflammatory arthritis. It’s characterized by sudden and recurrent attacks of painful swelling of one or more joints. Attacks may last for several days or just a few hours. Between attacks, palindromic rheumatism symptoms completely disappear and joints go back to normal, with no lasting damage, which can help distinguish it from RA. However, about a third of the people who have palindromic rheumatism will go on to develop RA, which does cause permanent joint damage.
How Rheumatologists Diagnose RA (and What You Can Do to Help)
Findings from a physical exam and medical history are important factors in diagnosing RA, say experts. Common RA symptoms include:
- Joints that feel tender, warm, or swollen for six weeks or more
- Multiple joints can be affected
- Joint pain that is commonly symmetrical
- Joint stiffness, especially first thing in the morning that lasts for an hour or more
- Fatigue
- Low-grade fever
- Loss of appetite
While many of these symptoms can occur with other diseases, infections, or injuries, there are subtle traits unique to RA that can help doctors make the diagnosis.
“Pain, swelling, and stiffness in smaller joints — in the hands, toes, and elbow, for example — as opposed to one or two bigger joints, like the knee and hip, usually indicates a pattern more likely to be RA,” says Dr. Husni. Pain from RA is usually more symmetric in nature, occurring on both sides of the body. When you injure yourself or have an overuse injury, however, pain usually occurs in just one joint. Joint stiffness can occur with injuries or other conditions, but stiffness with RA typically occurs in the morning and can be overwhelming, explains Dr. Husni. “It’s not a joint stiffness that passes after a few minutes, but more like you can’t even move the covers to get out of bed.”
In addition to a physical exam and taking your history, your rheumatologist will order blood tests to help diagnose RA. They are used to look for high levels of inflammation in the body, as well as certain antibodies that can be seen in many but not all cases of RA, such as rheumatoid factor or anti-CCP antibodies. Imaging studies, such as X-rays or MRI scans, can also help detect RA or gauge its severity.
If rheumatoid arthritis is diagnosed, a rheumatologist will partner with you to develop a treatment plan that works best for you. That’s what happened with Liang Harris. After getting diagnosed with RA, she went to her mother’s rheumatologist and started treatment. It took about six months to find the right combo of medications, she recalls, but now — 11 years after being diagnosed with rheumatoid arthritis — she and her rheumatologist work together to keep her RA under good control.





