No two patients with psoriatic arthritis (PsA) are dealing with the exact same set and severity of symptoms and issues. Some people may experience more skin-related symptoms, while others may be more bothered by joint pain, enthesitis, fatigue, or nail changes. But when it comes to signs your psoriatic arthritis is getting worse, there’s one piece of advice all people with PsA should follow: Don’t wait to alert your physician about any new or worsening symptoms. Take note of any changes in your health and schedule a visit as soon as possible.
It’s always better to inform your physician so they can determine if the worsening symptoms are related to PsA, says Elizabeth Schulman, MD, a rheumatologist at Hospital for Special Surgery in New York City. “We would rather know now than have you wait.”
From more frequent flares and fatigue to eye inflammation and nail pitting, here’s a look at some common symptoms that may point to psoriatic arthritis progression and your PsA getting worse.
Read on to know what to watch for — and how to work with your health care provider to get your PsA back on track.
How Your Doctor May Determine If Your Psoriatic Arthritis Is Getting Worse
If you are having worsening PsA symptoms, it’s important to let your rheumatologist know right away. You’ll likely need an in-person visit so your doctor can order tests and evaluate your disease activity.
To figure out if your psoriatic arthritis is progressing, your physician will likely use some of the following evaluations, along with a physical exam, to check for worsening skin psoriasis and joint mobility:
- Joint count test: This requires the doctor to examine certain joints (typically a set of 28 joints in your fingers, arms, and legs) for swelling, tenderness, or pain.
- Psoriasis Area and Severity Index (PASI) score: This assessment measures the severity and extent of psoriasis in four areas of the body: head and neck, upper limbs, chest and back, and lower limbs.
- Patient-reported outcomes (PROs): These are various surveys patients take about their symptoms and how their disease is impacting their daily life. They can tell your doctor about the pain from your psoriatic arthritis, as well as how it is impacting your everyday function and disability.
- Points of enthesitis: Enthesitis is inflammation at places where tendons and ligaments attach to bone (such as the Achilles heel or elbow). It is common in certain forms of inflammatory arthritis like PsA.
- Bloodwork: There are several blood tests, such as erythrocyte sedimentation rate, C-reactive protein, and plasma viscosity, that can track elevated inflammation markers.
- Image testing: This evaluation can include X-rays, ultrasounds, CT scans, or MRIs to check for joint damage.
Understanding Disease Activity
With a condition like psoriatic arthritis that affects many different parts of the body and causes a range of symptoms, there’s no one clear test that can tell you and your doctor how you’re doing. It’s very different than, say, getting a blood test that reveals your blood sugar level. Your doctor needs to look at a number of different measures to get a full picture of how your active your PsA is and how it is affecting your health.
There are many different ways to evaluate disease activity in psoriatic arthritis, but one that is becoming increasingly popular is called minimal disease activity. This score takes into account many of the evaluations listed above, including:
- Number of tender joints
- Number of swollen joints
- A psoriasis area and severity index (PASI) score
- Your own assessment of pain
- Your own assessment of disease activity
- Your own assessment of everyday function and disability
- Number of points of enthesitis
This helps ensure that doctors and patients are taking a broad look at how PsA affects someone’s health, so your doctor isn’t just looking at your skin plaques or the amount of joint pain, but also your own evaluations (patient-reported outcomes) of how your condition is affecting your daily function.
By using a well-rounded measure like minimal disease activity to monitor PsA, you and your doctor can identify if your current PsA treatment plan is helping to improve your symptoms and consider making a change if it’s not.
As soon as you start to notice changing or worsening symptoms, track their frequency and severity in a journal. This can give your doctor some background information to further help with their diagnosis.
You can also use our ArthritisPower app to track your symptoms and disease activity and share your results with your doctor.
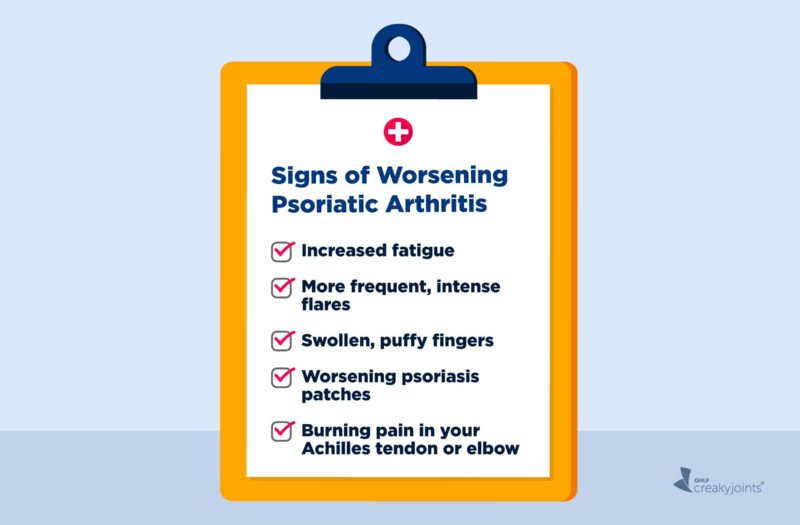
Signs Your Psoriatic Arthritis May Be Getting Worse
You need to work with your health care provider to determine whether and to what degree your psoriatic arthritis is getting worse. But looking out for these common clues can help you have a more informed conversation with your doctor so you can figure out what’s going on and how to treat it.
More trouble with daily activities
Is prolonged morning stiffness making it harder than normal to get up, get dressed, and get ready for work? Are you struggling to do daily activities like cooking, cleaning, or exercising because of joint pain or fatigue? Do you have less stamina?
If your PsA is progressing — and you have more inflammation, joint pain, and stiffness — there can be “a ripple effect that’s proportionate to your daily activities,” says Dr. Schulman.
You should let your rheumatologist know if you’re having more trouble with daily activities. “We really care about patients’ activity of daily living and their participation in their work, personal life, and the things they like to do,” Dr. Schulman says.
Increased fatigue
If fatigue is forcing you to nap in the middle of the day or preventing you from completing your work on time, it’s important to meet with your health care provider to tease out the underlying cause of your fatigue, says Dr. Schulman.
Fatigue is a common and challenging part of living with PsA, affecting 30 to 40 percent of patients. But just because it’s common doesn’t mean it’s normal or something you should accept. Fatigue can also be a sign that your PsA is active and/or not well-controlled. An observational study of 1,062 patients with psoriatic arthritis, published in the Journal of Rheumatology, found that fatigue was often driven by indicators of disease progression, including swollen and tender joints, elevated CRP, disease duration, and chronic pain.
“When your body is inflamed, it’s chronically fighting itself,” explains Dr. Schulman. “The cytokines [immune system proteins] that are stimulated [during chronic inflammation] can cause a patient to feel malaise and fatigue.” If pain and stiffness is interfering with your sleep, or causing early morning wakening, that can also contribute to your fatigue, she adds.
Read more here about coping with fatigue in psoriatic arthritis.
More frequent (or intense) flares
If you’re having more frequent psoriatic flares, or if your flares are keeping you in bed or affecting multiple joints, it’s really important to let your rheumatologist know, says Dr. Schulman.
There’s no set definition of a PsA flare, but it can include joint pain and swelling, an increase in psoriasis skin plaques, and fatigue or brain fog. It typically lasts a few days to a few weeks.
“There are no consistent guidelines to how many flares are acceptable — some would say that no flares are acceptable,” says Dr. Schulman. It’s different for everyone, and each patient has a different threshold, but an uptick in the frequency or severity of flares could indicate that your medication isn’t working well anymore, she explains.
Flares aren’t just frustrating or inconvenient: They are a sign you have unchecked inflammation that can be harming your health. “Prolonged and frequent flares eventually will cause joints damage and deformities,” adds Zhanna Mikulik, MD, a rheumatologist and immunologist at the Ohio State University Wexner Medical Center.
Worsening psoriasis patches
“It’s important to think of PsA as one disease with various organ involvement,” says Dr. Schulman. This means that if your skin is flaring, but your joints and spine are stable, it still may indicate a progression of your disease.
You may notice more body surface involvement, lesions that aren’t going away with creams or injectables, or thicker, worse lesions, explains Mona Gohara, MD, Associate Clinical Professor of Dermatology at Yale School of Medicine in New Haven, Connecticut.
If you are having more skin flares, you may need a change in therapy. “Some medications work better for the skin and don’t work as well for the joints, so it must be a collaborative effort with the dermatologist, rheumatologist, and patient,” says Dr. Schulman.
Back pain
Back pain is very common, so back or neck pain alone isn’t necessarily cause for alarm, especially if you know your tweaked your back doing housework, say, or feel sore from a long car ride. But many people with psoriatic arthritis may not realize that the spine can also be affected by inflammation.
So don’t shrug off consistent back or neck pain, because it can be part of the disease and present later on as PsA progresses, says Dr. Schulman.
As part of the PsA disease spectrum, patients can get specific types of back pain that are typically inflammation-driven, she adds, noting that signs of inflammatory back pain include:
- Morning stiffness that gets better with activity
- Alternating buttock pain
- Pain that wakes you up early in the morning
- Pain that gets better after taking non-steroidal anti-inflammatory drugs (NSAIDs)
Burning pain in your Achilles tendon or elbow
If you’re suddenly experiencing pain in your Achilles tendon, near the bottom of your feet (plantar fascia), or in your elbow (epicondyle), it could mean that you’re PsA is getting worse.
Inflammation of the enthesis, where a tendon or ligament attaches to bone, impacts roughly half of people with psoriatic arthritis, according to the journal Seminars in Arthritis and Rheumatism. It’s often caused by a chronic state of inflammation. It can be brought on by microtrauma, but it can also be a sign of disease progression, says Dr. Schulman.
Read more about enthesitis.
Swollen and puffy fingers
A classic finding in uncontrolled PsA is dactylitis — painful, red, and hot swelling that can affect an entire digit (fingers or toes) rather than just a knuckle. “The swollen fingers and toes occur due to soft tissue inflammation,” explains Dr. Mikulik.
As the nickname “sausage fingers” implies, the swelling and deformity is often obvious. However, this is not always the case, says Dr. Schulman. She suggests taking note if your rings are more difficult to get on and off, or if you’re suddenly experiencing problems making a fist.
“Acute or chronic deformity can absolutely signal that your disease is not controlled, or is flaring,” says Dr. Schulman.
Read more about dactylitis.
Changes in your nails
A 2020 study in the Journal of Rheumatology linked nail psoriasis in patients with PsA to worse disease activity, quality of life, and work productivity than in those without nail involvement.
“Nail pitting [uneven surface indents] or fingernail changes can be an indication that you have worsening PsA,” says Dr. Schulman. This can happen even if you only have skin involvement or only have joint involvement.
In addition to pitting, Dr. Mikulik says to take note of any changes in nail shape, yellow-brown color nails, or nails that separate from the nail bed (onycholysis).
Hearing loss
Are you having trouble hearing or struggling with balance problems? This may be related to unmanaged PsA, according to a 2017 study of mostly male PsA patients published in the Journal of Rheumatology. Researchers found that 60 percent of patients experienced abnormal hearing loss and/or inner ear damage compared to 8 percent of controls.
However, Dr. Schulman says hearing loss is not something brought up by her patients, and further research is needed to prove the direct correlation between progression of hearing loss as a marker of worsening disease.
Eye inflammation
The same systemic inflammation that affects your joints can also affect your eyes, leading to a red, painful eye with visual changes, says Dr. Schulman. In fact, uveitis, or an inflammation of the middle layer of your eye, occurs in 7 to 20 percent of people with PsA, according to a 2019 study published in the journal Psoriasis: Targets and Therapy.
If you experience uveitis, you should have an urgent ophthalmologist evaluation, says Dr. Schulman. If steroid eye drops don’t work to lower your eye inflammation, or if you’re experiencing recurring bouts of uveitis, it likely means that your disease is not optimally controlled.
It may even warrant a change in therapy, she adds, since some medications can help with joint and skin involvement but don’t work for eye inflammation.
Read more about uveitis.
Track Your Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Sign up here.
Amor-Dorado JC, et al. Investigations into Audiovestibular Manifestations in Patients with Psoriatic Arthritis. The Journal of Rheumatology. October 2014. doi: https://doi.org/10.3899/jrheum.140559.
Fotiadou c, et al. Psoriasis and uveitis: links and risks. Psoriasis: Targets and Therapy. August 28, 2019. doi: https://doi.org/10.2147/PTT.S1791.
Interview with Elizabeth Schulman, MD, Rheumatologist at Hospital for Special Surgery
Interview with Mona Gohara, MD, Associate Clinical Professor Dermatology at Yale School of Medicine
Interview with Zhanna Mikulik, MD, Rheumatologist and Immunologist at the Ohio State University Wexner Medical Center
Kaeley GS, et al. Enthesitis: A hallmark of psoriatic arthritis. Seminars in Arthritis and Rheumatism. August 2018. doi: https://doi.org/10.1016/j.semarthrit.2017.12.008.
Lozada CJ. What is the role of arthrocentesis in the diagnosis of osteoarthritis (OA)? Medscape. October 12, 2020. https://www.medscape.com/answers/330487-44933/what-is-the-role-of-arthrocentesis-in-the-diagnosis-of-osteoarthritis-oa.
Mease PJ, et al. Association of Nail Psoriasis With Disease Activity Measures and Impact in Psoriatic Arthritis: Data From the Corrona Psoriatic Arthritis/Spondyloarthritis Registry. The Journal of Rheumatology. October 2020. doi: https://doi.org/10.3899/jrheum.190923.
Oakley A. PASI score. DermNet NZ. 2009. https://dermnetnz.org/topics/pasi-score.
Skougaard M, et al. In Psoriatic Arthritis fatigue is driven by inflammation, disease duration, and chronic pain: An observational DANBIO registry study. The Journal of Rheumatology. July 2019. doi: https://doi.org/10.3899/jrheum.181412.