When dealing with a chronic disease like rheumatoid arthritis (RA), no two days are exactly alike. Some days, you may have minimal pain and be able to function similarly to how you did before you had RA. Other days, you may barely be able to get out of bed due to swollen, stiff joints and fatigue. And although days like that unfortunately come with the territory, it’s important to be able to tell the difference between signs of a particularly bad flare and signs that your rheumatoid arthritis is getting progressively worse.
When you talk about rheumatoid arthritis “getting worse,” that could mean two things, says Beth Ilene Wallace, MD, MSc, an Assistant Professor in Internal Medicine at the University of Michigan and rheumatologist at the VA Ann Arbor Healthcare Center. “First, we could mean worsening RA symptoms,” she says. “Second, we could mean RA disease progression, [which] could mean tissue damage related to inflammation, or inflammation and related damage in other tissues where the patient hasn’t previously had problems.”
Worsening RA symptoms and disease progression can go hand in hand, but you can also have RA-related inflammation when symptoms are stable or minimal, she adds.
Here are some common signs that your RA may be getting worse — and how to work with your health care provider to get your disease back under control.
“Identifying worsening rheumatoid arthritis early will be better for your health, comfort, and quality of life,” says Nilasha Ghosh, MD, rheumatologist at Hospital for Special Surgery in New York City. “Untreated disease can lead to complications such as irreversible joint damage and deformity. The goal is to stop the inflammation before it gets to this point.”
How Your Doctor May Determine If Your Rheumatoid Arthritis Is Getting Worse
If you suspect you are having worsening RA symptoms, it’s important to let your rheumatologist know right away. You’ll likely need an in-person visit so your doctor can order tests and evaluate your disease activity.
Your rheumatologist will likely ask about your pain and function and check bloodwork for inflammation markers. “These assessments can be tracked over time to help your doctor monitor your rheumatoid arthritis [disease] activity,” says Dr. Wallace.
Your rheumatologist will use a variety of tools and tests to track your RA and see if things are improving, worsening, or staying the same. This may include:
- Physical exam: This will likely involve checking the range of motion of your joints, as well as the way your joints look and function.
- Joint count test: This requires the doctor to examine certain joints (typically a set of 28 joints in your fingers, arms, and legs) for swelling, tenderness, or pain.
- Patient-reported outcomes (PROs): These are various surveys patients take about their symptoms and how their disease is impacting their daily life. They can tell your doctor about the pain from your rheumatoid arthritis, as well as how it is impacting your everyday function and disability.
- Bloodwork: There are several blood tests, such as erythrocyte sedimentation rate, C-reactive protein, and plasma viscosity, that can track elevated inflammation markers.
- Image testing: This evaluation can include X-rays, ultrasounds, CT scans, or MRIs to check for bone damage or new or worsening symptoms outside of the joints. For example, if you have a worsening cough or shortness of breath, you may need a CT scan of your chest to look for lung problems associated with RA, explains Dr. Wallace.
Understanding Disease Activity and Remission
With a condition like rheumatoid arthritis that affects many different parts of the body and causes a range of symptoms, there’s no one clear test that can tell you and your doctor how you’re doing. It’s very different than, say, getting a blood test that reveals your blood sugar level. Your doctor needs to look at a number of different measures to get a full picture of how your active your RA is and how it is affecting your health.
There is currently no cure for RA, but you can achieve a state where your disease is unlikely or less likely to cause further joint damage or other serious health problems. This is known as 1) low disease activity; or 2) remission.
Low disease activity and remission are different from each other, but similar: Remission means that there is very low or even no active disease, as measured by blood tests and a physical exam. Low disease activity means that your disease activity is low and is keeping your symptoms under control and helping you maintain a good quality of life.
Get our Patient’s Guide to Rheumatoid Arthritis Testing and Monitoring to learn more.
If you’re experiencing changing or worsening symptoms, it can be a sign that your disease activity is increasing and you may need a change in your treatment plan.
As soon as you start to notice changing or worsening symptoms, track their frequency and severity in a journal. This can give your doctor some background information to further help with their diagnosis.
You can also use our ArthritisPower app to track your symptoms and disease activity and share your results with your doctor.
Signs Your Rheumatoid Arthritis May Be Getting Worse
You need to work with your health care provider to determine whether and to what degree your rheumatoid arthritis is getting worse. But looking out for these common clues can help you have a more informed conversation with your doctor so you can figure out what’s going on and how to treat it.
More visibly swollen and tender joints
Perhaps the easiest way to tell if your RA is getting worse is if the number of visibly swollen and tender (another word for painful) joints is increasing. Rheumatoid arthritis commonly first affects joints in the fingers and toes, and may start to affect more joints — such as the wrists, elbows, shoulders, or knees — over time.
Although your physician regularly checks your joints with physical exams, and can note which joints are affected, Dr. Ghosh says it can be helpful for you to give your input as well. “It is a good idea to monitor which of your joints are affected by pain, stiffness, and/or swelling, as these may change from day to day and may increase over time, especially if your disease is undertreated.”
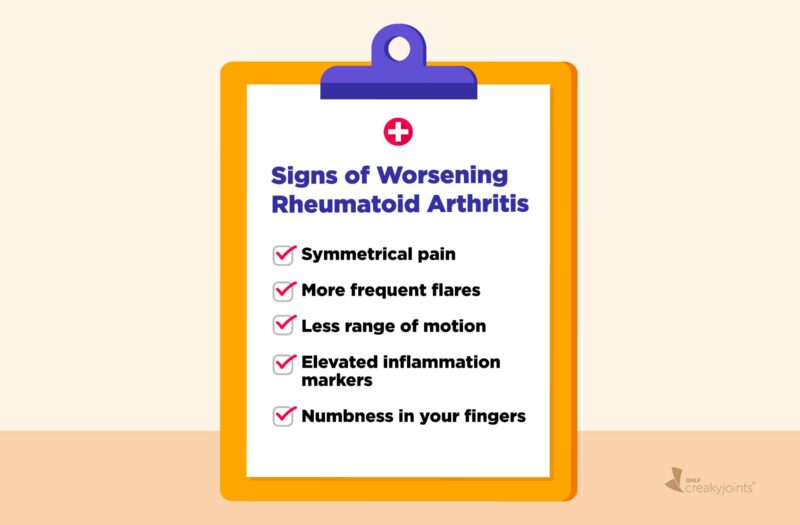
Symmetrical pain
In the early stages of RA, when only a few joints may be affected, you may not experience pain on both sides of the body. As the disease progresses, however, pain felt in a joint on one side of the body will likely be felt in the same joint on the other side. That said, the degree of pain may be different on each side, so it’s important to pay attention to pain location rather than just pain severity.
More frequent flares
When your RA is under control, you’ll likely have flares — a period of days or weeks where symptoms are worse than normal — one to two times per year, says Dr. Wallace. In comparison, she notes, people with worsening symptoms may have these flares every month, or even several times a month.
“If you are experiencing flares more frequently, usually manifesting as increased pain, stiffness, and swelling, your RA could be getting worse,” adds Dr. Ghosh.
Increased stiffness and difficulty bending your joints
Stiffness that accompanies RA is most prominent after long periods of inactivity, such as in the morning after waking up, explains Dr. Ghosh.
If your stiffness becomes prolonged, or doesn’t improve with activity, it’s important to report this symptom to your doctor. “Take note of how many minutes, or hours, your stiffness typically lasts before you feel loosened up,” says Dr. Gosh.
Less range of motion
Have you noticed that your fingers deviate off to the side, or that you can no longer bend or straighten certain joints like the neck, fingers, wrists, or elbows?
As RA progresses, it causes joint damage that leads to irreversible deformities and/or contractures. “If you notice that you cannot move your joints as much or as easily as before, even if you don’t have swelling or pain, your RA may be getting worse,” says Dr. Ghosh.
Changes in the way joints look or function, which do not improve with changes in RA treatment, can be a sign of disease progression, says Dr. Wallace.
Rheumatoid nodules
According to the American Osteopathic College of Dermatology, roughly 25 percent of people with RA develop rheumatoid nodules, or firm or doughy bumps on the joints. Nodules are particularly common in the upper extremities, explains Dr. Ghosh. While this may be due to certain medications, feeling nodules over your hand, forearms, and elbows can also signal high disease activity, she says.
Read more about rheumatoid nodules.
Elevated inflammation markers
Higher levels of inflammatory markers, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), can signify worsened RA, says Dr. Ghosh.
According to the University of Rochester Medical Center, a CRP level over 10 milligrams/liter and an ESR above 100 millimeters/hour indicate inflammation. Your doctor, however, will likely compare your numbers against your last blood sample to determine what the test results mean for you. Keep in mind: You can also have elevated inflammation markers when you’re sick with an infection or because of other health conditions, so they’re not necessarily indicative of RA disease progression all by themselves.
Feeling more fatigued or weaker
Fatigue is a common symptom of RA, as well as a possible side effect of some of the medications used to treat it. Fatigue can also be an indication of high inflammation throughout the body. “RA fatigue could also lead to poor sleep and mood changes, which will also affect one’s energy,” says Dr. Ghosh.
Having more trouble with daily activities
“RA affects joints that are important for doing our activities of daily living,” says Dr. Ghosh. This is why fine motor skills like holding a coffee cup, grasping kitchen utensils, gripping jars, turning a doorknob or faucet, or buttoning/unbuttoning clothes can be challenging. If these tasks are becoming harder, or not easier as the day progresses, you’ll want to notify your rheumatologist.
Numbness/tinging in your fingers
Unmanaged inflammation in the wrist joints can cause nerve compression, resulting in weakness, tingling, and numbness in the hands and fingers. “While most cases of carpal tunnel syndrome are not related to an inflammatory condition, worsening RA can precipitate numbness and tingling in some fingers,” says Dr. Ghosh.
Read more about the connection between carpal tunnel and arthritis.
Changes in other areas of the body
Due to the inflammatory nature of RA, it can affect other parts of the body, such as the eyes, lungs, and heart. Untreated or undertreated inflammation in RA has been linked to cardiovascular disease and certain cancers, says Dr. Ghosh, adding that “this risk can go down once the RA is being treated appropriately.”
In other words, don’t dismiss symptoms that at first may seem unrelated to RA, say Dr. Wallace. “For example, a person who has developed lung problems related to their rheumatoid arthritis may develop shortness of breath when they climb stairs, or a cough that won’t go away.”
Track Your Symptoms with ArthritisPower
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Sign up here.
Watch: Switching Rheumatoid Arthritis Medications
This video is part of an educational project from researchers at Yale University, Berkshire Medical Center, Carnegie Mellon University, Hospital for Special Surgery, CreakyJoints and the Global Healthy Living Foundation, and ArthritisPower. It was made possible with support from the Rheumatology Research Foundation. Watch more videos from this series here.
Bhandari B. Prevalence of Cancer in Rheumatoid Arthritis: Epidemiological Study Based on the National Health and Nutrition Examination Survey (NHANES). April 28, 2020. doi: https://doi.org/10.7759/cureus.7870.
C-Reactive Protein (Blood). University of Rochester Medical Center. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=c_reactive_protein_serum.
Erythrocyte Sedimentation Rate. University of Rochester Medical Center. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=erythrocyte_sedimentation_rate.
Interview with Beth Ilene Wallace, MD, MSc, a rheumatologist at the VA Ann Arbor Healthcare Center
Interview with Nilasha Ghosh, a Rheumatologist at Hospital for Special Surgery
Rheumatoid Nodules. American Osteopathic College of Dermatology. https://www.aocd.org/page/RheumatoidNodules.