Lupus is an autoimmune disease that occurs when your immune system attacks your own tissues and organs. The inflammation from lupus can affect different parts of the body, including the kidneys, the brain and central nervous system, the heart, lungs, blood vessels, and more.
Lupus affects different people differently. Symptoms can come on suddenly or build up over time. They may be mild or severe. Many cases of lupus are characterized by flares, where symptoms temporarily worsen and then improve or disappear for a period of time.
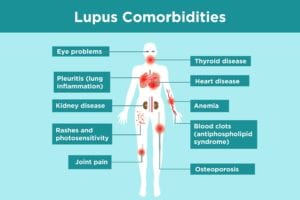
There are many different types of lupus. The most common is systemic lupus erythematosus (SLE), which accounts for approximately 70 percent of all cases of lupus, according to the Lupus Foundation of America. Patients with SLE have many comorbidities, a U.K. study found. Discoid lupus erythematosus only affects the skin. Drug-induced lupus is a form of lupus caused by certain medications. Read more basic facts about lupus.
Lupus complications are more likely to occur when lupus isn’t well-controlled, which is why a mainstay of lupus treatment is trying to prevent complications. Today, more treatment options than ever are available for managing lupus, with many others currently being studied. The right treatment for you depends on which type of lupus and which symptoms you have. Common medications for lupus include nonsteroidal anti-inflammatory drugs (NSAIDs); hydroxychloroquine (Plaquenil); corticosteroids; immune-suppressing drugs such as azathioprine, mycophenolate mofetil, and methotrexate; and certain biologics approved to treat lupus.
The most important thing you can do right away as a lupus patient is find a health care provider you trust, says Jill Buyon, MD, a rheumatologist and director of the Lupus Center and director of Division of Rheumatology at NYU Langone Health in New York City.
Once you read through this list of lupus complications, bring up any questions or concerns you have with your doctor. You may need to create a health care team of different specialists —such as seeing a rheumatologist, a cardiologist, and a nephrologist — or facilitate better communication among them to ensure you’re getting optimal care for your lupus and its comorbidities.
Lupus Comorbidities
1. Lupus and the Heart
About 50 percent of lupus patients experience heart complications, according to the Hospital for Special Surgery in New York City. “Inflammation from lupus puts you at increased risk of cardiovascular disease,” says Lisa Criscione-Schreiber, MD, associate professor of medicine and rheumatology training and program director chair for the Program for Women in Internal Medicine in the Duke Department of Medicine in Durham, North Carolina.
In fact, a meta-analysis published in the journal Seminars in Arthritis and Rheumatism revealed at least a two-fold increased cardiovascular risk for SLE patients. “The most common cardiac complication of lupus is atherosclerosis [when plaque clogs the arteries] and heart attacks,” says Christopher Collins, MD, a rheumatologist at MedStar Washington Hospital Center in Washington, DC. While early stages of atherosclerosis don’t have many symptoms, as plaque builds up and starts to block the artery it can cause:
- Chest pain
- Fatigue
- Shortness of breath
- Muscle weakness in your leg (from lack of circulation)
- Pain in your leg, arm, or anywhere that has a blocked artery
Heart attacks can happen at a younger age in lupus patients than in the general population. “Lupus patients are under-recognized as having this independent risk factor,” says Dr. Collins. Physicians and patients may dismiss chest pains among patients with lupus, thinking they’re too young to have a heart attack.
Lupus heart complications also include pericarditis, which is inflammation in the pericardium, the membrane that surrounds the heart. Symptoms include breathlessness and chest pain when you breathe deeply, cough, or swallow.
Lupus patients may need additional treatment, such as blood pressure or cholesterol medications, to manage heart disease risk factors. Exercising regularly, eating healthy, and quitting smoking can help reduce some risk factors of heart disease.
2. Lupus and Antiphospholipid Antibody Syndrome
Approximately 50 percent of people with lupus develop antiphospholipid antibodies. These antibodies are directed against the fatty parts of your cell membranes. One of these antibodies, the lupus anticoagulant, predisposes you to developing blood clots, which can lead to stroke and heart attack.
Antiphospholipid antibodies don’t necessarily correlate with lupus disease activity, which means that they can cause problems even if your lupus is controlled. Many people with antiphospholipid antibodies have a purple or reddish lacy pattern just under their skin on the arms and legs, known as livedo. However, livedo is also associated with other blood vessel diseases, so it doesn’t necessarily mean you have antiphospholipid antibodies.
People who develop a complication from antiphospholipid antibodies, such as a blood clot or a miscarriage, are considered to have antiphospholipid antibody syndrome (APS). APS usually requires medication to help prevent blood clotting, such a blood thinner or daily baby aspirin.
3. Lupus and the Lungs
Lung involvement over the course of lupus is very common; it affects about half of patients, according to the John Hopkins Lupus Center. The most frequent lung problem that affects people with lupus is inflammation around the pleura, a membrane that covers the outside of the lungs and inside of the chest cavity. This is called pleuritis, also known as pleurisy. Symptoms of pleurisy include severe, sharp stabbing pain that worsens when you take a deep breath, cough, sneeze, or laugh. You may have shortness of breath. Pain from pleurisy occurs in 40 percent to 60 percent of people with lupus, says the Lupus Foundation of America.
Treatment for pleuritis includes steroids like prednisone, which can also help relieve lupus flares, says Dr. Collins. Immunosuppressant medications like methotrexate may also be prescribed to help prevent the condition. Sometimes the two medications are taken simultaneously, says Dr. Collins.
4. Lupus and the Blood
Blood is made of many parts. Those that are most often affected by lupus are the red blood cells, the white blood cells, and the platelets. Anemia, explained below, affects about half of all people with active lupus.
Anemia of Chronic Disease
The most common blood disorder that affects lupus patients is called anemia of chronic disease. Anemia means you have too-low levels of circulating red blood cells or hemoglobin, the part inside red blood cells that carries oxygen from the lungs to the body tissues. It can be associated with many conditions, including lupus.
Fatigue is the most common symptom of anemia. Treatment of anemia in lupus depends on its cause. If your anemia is due to inflammation, it’s often treated with prednisone. “That’s why at every visit, every three months or so, you’ll have your blood analyzed for those silent aspects of blood activity that you don’t have symptoms for,” says Dr. Collins.
Hemolytic Anemia
Lupus patients can also have hemolytic anemia, a disorder where red blood cells are destroyed faster than they can be made. Symptoms include weakness, dizziness, abnormal paleness, and dark-colored urine. Treatment varies depending on the cause of the illness but may include blood transfusion or taking the biologic rituximab (Rituxan).
5. Lupus and Skin
Most people with lupus experience some sort of skin involvement during the course of their disease.
Malar Rash
One telltale sign of lupus — which may even help patients get diagnosed — is the presence of a butterfly-shaped rash on your nose and cheeks, called a malar rash. It’s red or purplish in color. It covers the cheeks and bridge of your nose, but usually not the rest of your face. The rash can be raised or flat. “It’s often confused with rosacea,” says Dr. Buyon. Many health conditions can cause the rash, including lupus and other autoimmune disorders.
Discoid Lupus
Another lupus skin problem that’s a complication of lupus is called discoid lupus. It’s a chronic autoimmune disease that affects the skin that causes a rash that is red, scaly, thick, and round. It gets its name from the coin-shaped lesions it produces. The rash can appear on the scalp and face and can be confused with psoriasis, says Dr. Buyon. The exact cause of discoid lupus is unclear. It may be an autoimmune disease, with genetic and environmental triggers. It doesn’t pass from person to person.
These skin conditions can be treated with topical steroid creams and the medication hydroxychloroquine, says Dr. Criscione-Schreiber.
Photosensitivity
People with lupus also experience photosensitivity, in which your skin reacts to ultraviolet rays from sunlight and other light sources like indoor fluorescent light. Having photosensitivity from lupus can cause rashes, fever, fatigue, and joint pain. Each person handles exposure to ultraviolet rays differently though. Prevent skin complications by reducing sun exposure, applying sunscreen, and wearing wide-brimmed hats and sun protective clothing.
6. Lupus and Joints
More than 90 percent of people with lupus will experience joint and/or muscle pain at some point during the course of their illness, according to the Lupus Foundation of America. More than half of people who develop lupus mention joint pain as their first symptom.
Lupus often causes people to develop arthritis or joint pain. Lupus causes inflammation throughout the body, including the joints. But the form of arthritis trigged by lupus is different than that caused by rheumatoid arthritis. Lupus arthritis is much less severe than rheumatoid arthritis: Lupus arthritis doesn’t damage the joints long-term the way other kinds of inflammatory arthritis do, but it does cause pain in the joints. People with lupus also experience muscle aches and pain or have inflammation of certain muscle groups.
You can get joint pain relief from nonsteroidal anti-inflammatory medications (NSAIDs) such as ibuprofen or naproxen. You may also be given steroids like prednisone. “Medication really depends on the severity of the condition,” says Dr. Buyon. Ease joint stiffness with ice packs. Stay active with low-impact workouts like yoga or walking.
7. Lupus and Kidneys
It’s estimated that up to 60 percent of all people with lupus will develop kidney complications that require medical evaluation and treatment, says the Lupus Foundation of America. Lupus nephritis is a type of kidney inflammation and a common complication in people who have lupus. Kidney problems are two to three times more likely among African-Americans with lupus than Caucasians, according to Dr. Collins. You’re also more likely to have kidney conditions if your lupus is diagnosed at a younger age.
Symptoms of kidney problems include swelling in your ankle or lower leg, foamy or frothy urine, or blood in your urine.
However, the kidneys are amazing in their ability to compensate for problems in function. Chronic kidney disease may progress without symptoms for a long time until minimal kidney function is left. “That’s why at every visit I’m taking a urine sample because I’m looking for any early signs of kidney issues like protein in the urine,” Dr. Buyon says. Your doctor can do bloodwork to look for protein or blood cells in your urine and to make sure your kidneys are working well.
Lupus nephritis has no cure, so treatment involves controlling symptoms and trying to minimize further stress on the kidneys. This may entail taking medication to control blood pressure and following a special diet low in protein and salt. For severe lupus nephritis, you might take drugs that stop your immune system from attacking healthy cells. If lupus nephritis leads to kidney failure, you might need dialysis, a procedure which removes extra fluids and waste from your blood by filtering your blood through a machine. If your kidneys no longer work, you might need a new kidney from a donor.
8. Lupus and the Eyes
The eyes can also be target of lupus. Any structure of the eye can be involved in the disease. Many eye problems in patients with lupus stem from the drugs doctors use to treat lupus itself since they can impact the eye adversely.
Sjögren’s Syndrome
Sjögren’s syndrome can occur alone or in association with other autoimmune diseases, most commonly lupus and rheumatoid arthritis. This autoimmune disease attacks and inflames moisture-producing cells like the salivary and tear glands. Symptoms include dry eyes and dry mouth. “Many patients have both lupus and Sjögren’s syndrome,” says Dr. Buyon. “I see it somewhat commonly. They can exist together.”
She suggests that lupus patients see an ophthalmologist annually, which is also required if you take Plaquenil (it can cause retinopathy, which is a known complication of the drug). Treatment depends on the parts of the body affected. Many people use over-the-counter eye drops and drink water more often to help prevent dry eye from Sjögren’s syndrome.
Discoid lupus
The eyelids can get irritated from discoid lupus, which can appear as a thickened rash over your eyelids. It has scaly, disc-shaped lesions. The lesions usually are treated with oral steroids.
Scleritis
The sclera is the tough, white outer coating of the eyeball. Scleritis causes the sclera to become inflamed, red, and painful. You can experience blurred vision and light sensitivity. This inflammation thins the sclera, which creates a weak area of the eye that can perforate. It can be treated with oral and topical steroids and NSAIDs.
Retinal vasculitis
Here, the blood supply to the retina in the back of the eye is decreased or limited. In turn, the retina tries to repair itself by developing new blood vessels. But the new blood vessels are fragile and weak. Blood and fluid can leak out of them, causing swelling in the retina.
9. Lupus and Thyroid Disease
The thyroid is a gland in your neck that helps controls your metabolism — the process by which your body uses energy. A study in the Journal of Clinical Rheumatology found that just over 6 percent of those with lupus tested had thyroid problems caused by autoimmune thyroid disease, compared to 2 percent in the general population. Hypothyroidism, a less active thyroid, is more common than hyperthyroidism, an overactive thyroid.
Hypothyroidism can cause weight gain, fatigue, depression, moodiness, and dry hair and skin. Hyperthyroidism can cause weight loss, heart palpitations, tremors, heat intolerance, and may lead to osteoporosis. Treatment for both thyroid problems aim to return your body’s metabolism to its normal rate. Hypothyroidism is usually treated with thyroid hormone replacement therapy. Hyperthyroidism is treated with anti-thyroid medications or radioactive iodine.
There are different explanations for the association between thyroid disease and lupus. They share demographic features, with young to middle-aged women more likely to have thyroid disease than men, as well as being more likely to have lupus. People with one autoimmune disease are at a higher risk for developing other ones. Since the thyroid gland can be a target for some lupus antibodies, it has been suggested that lupus antibodies and thyroid antigens may affect each other.
10. Lupus and Osteoporosis
Compared with the general population, people with lupus are at an increased risk for osteoporosis, which is an accelerated loss of bone mass. It can make you more prone to fractures. Osteoporosis and lupus are both more likely to occur in women, which is one explanation for the link.
But there are features of lupus itself as well as the drugs used to treat lupus that significantly increase osteoporosis risk. The disease itself can lead to bone loss. Lupus symptoms, such as pain and fatigue, may reduce physical activity in lupus patients, which can increase osteoporosis risk. And bone thinning is a side effect of the corticosteroid medications often used to treat inflammation in lupus.
Non-lupus related risk factors for developing osteoporosis include family history, using certain medications like corticosteroids, smoking, not getting enough calcium, or not getting enough physical activity. It’s a silent disease, which if undetected can progress without symptoms until a fracture happens.
Osteoporosis in lupus is treated with bisphosphonates, a group of medicines that slow down or prevent bone loss and strengthen bones. Weight-bearing exercises like walking, climbing stairs, and dancing can help maintain strong bone density. Don’t smoke. Ask your doctor about when and how often you should get bone mineral density tests, which can detect osteoporosis before a fracture happens.