Flares unfortunately come with the territory of managing chronic arthritis like ankylosing spondylitis (AS). AS is an inflammatory disease that primarily affects the spine and sacroiliac joints (which connect the spine to the pelvis); it can also impact other joints such as the ankles, knees, and neck, as well as cause inflammation of the entheses, which are connective tissues where tendons and ligaments attach to bone.
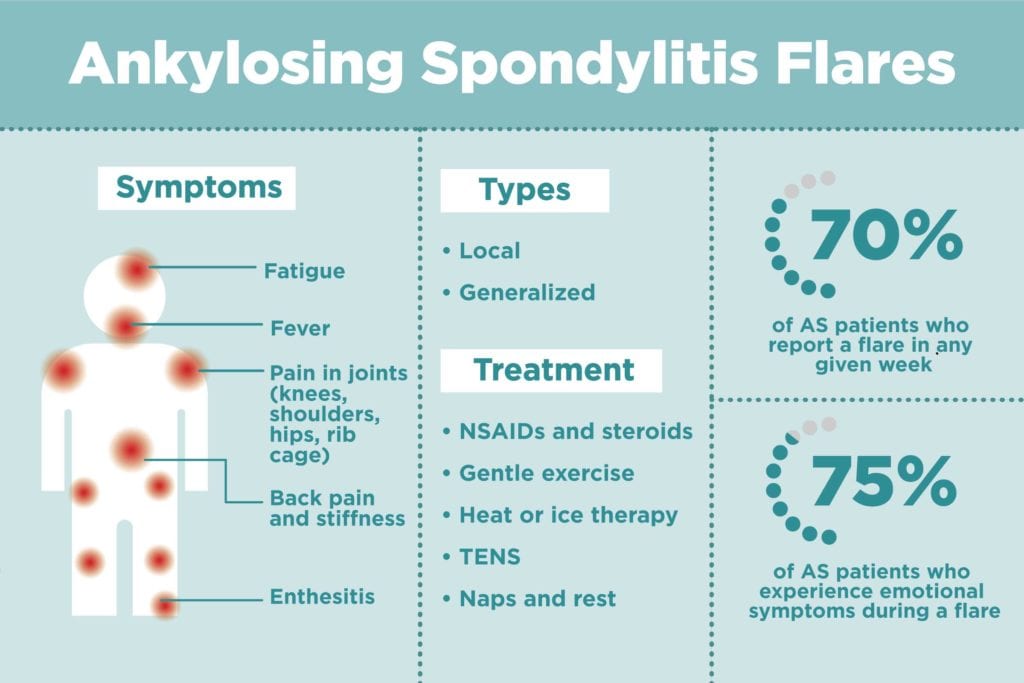
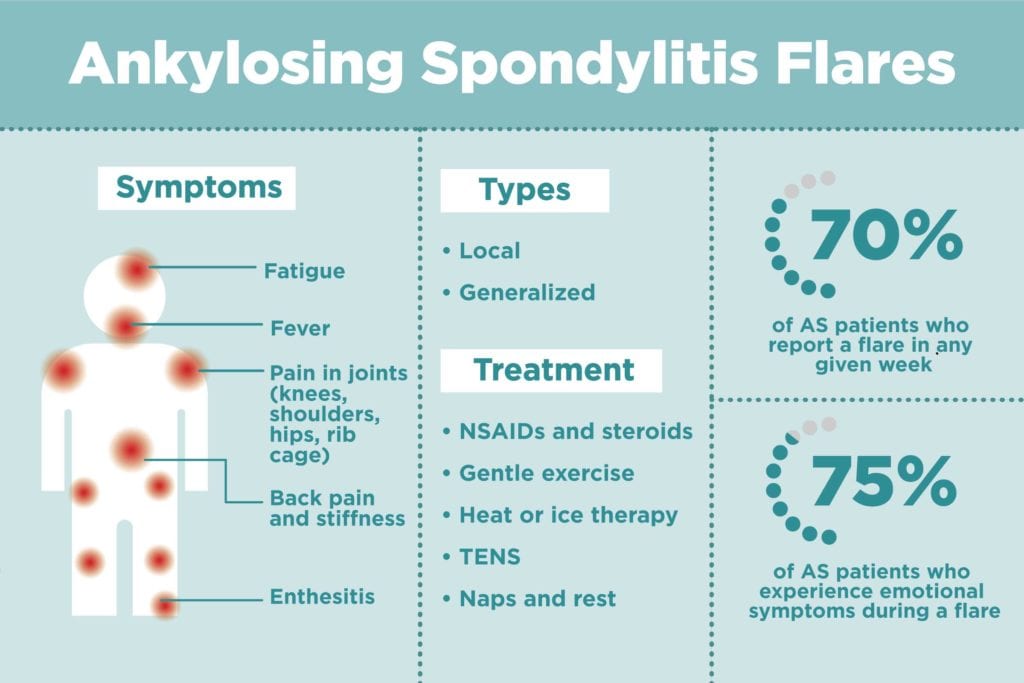
People with AS tend to have chronic lower back, pelvic, and hip pain that comes and goes; during a flare, it can feel significantly more intense and debilitating. Research indicates that flares in AS are very common. One study found that AS patients had about one flare a month; each flare lasted about two weeks. Another study found that 70 percent of AS patients reported a flare in any given week.
“Sometimes I literally wake up and I am in flare,” AS patient Tanya Greatorex told us on Facebook.
AS flares are physically awful, but they can also be just as emotionally taxing. In one study, researchers found that 75 percent of patients reported emotional symptoms, such as depression and anger, during an AS flare.
But with gentle exercise, stress management, listening to your body and the right medication treatment plan, you can get through these periods of flare-up. “You can’t prevent AS once it exists, but you can help to manage it and help prevent the long-term consequences,” says physical therapist Maura Daly Iversen, PT, DPT, SD, MPH, FAPTA , a spokeswoman for the American Physical Therapy Association (APTA). Here’s what to expect from ankylosing spondylitis flares, and how to deal with them.
Types of AS Flares
Based on patient surveys and self-reported experiences of flares, researchers characterize two main types of ankylosing spondylitis flares: localized and generalized.
- Localized flares are when symptoms affect one primary area, causing pain, immobility, and fatigue.
- Generalized flares are more severe and may affect multiple parts of the body. In addition to the above symptoms, they also include flu-like illness (fever, sweating); hot, burning joints; muscle spasms; and more sensitivity.
One study on AS flares found those who experienced generalized flares appear to have a more severe and active disease even when not in flare.
Ankylosing Spondylitis Flare Symptoms
Back pain and stiffness
As with many types of inflammatory arthritis, a flare is marked by the increase of normal disease symptoms. “If a patient experiences worsening joint or back pain lasting for more than a few days, then it is likely a flare,” says rheumatologist Joan Appleyard, MD, an assistant professor of medicine in the Division of Immunology, Allergy, and Rheumatology department at the Baylor College of Medicine in Houston. As Greatorex told us, AS pain is often worse first thing in the morning because you haven’t moved around much all night so your joints stiffen up. (Read more about how to manage back pain at night from ankylosing spondylitis here.)
Fatigue
As the AS flare takes its toll, you might feel completely wiped out. “With the fatigue it brings about, I find I nap a couple of times a day,” Greatorex says.
Pain in other joints
Although the pain might be centralized in your lower back, it can also affect other joints during a flare. “With AS you can have enthesitis, or an inflammation of the insertion of the tendon onto the bone, typically at your ankle joint or at your knee joint,” Iversen says. You may also have neck pain or pain in your rib cage — known as costochondritis — as well.
Depression
In one study, 75 percent of patients noted that emotional symptoms such as depression were part of their flare symptoms. Chronic pain can be mentally as well as physically debilitating.
Fever
Fever can be part of AS flares, but if you do have a fever, make sure you call your doctor, as it could be something else. “Systemic symptoms such as fever could signal an underlying infection,” Dr. Appleyard says. “Patients taking biologics [a class of medication used to treat AS] are at increased risk of infection and should seek medical attention immediately if they have a fever or other symptoms of infection such as chills, sweats, or weight loss. Never assume that these symptoms are due to a disease flare.”
Causes of AS Flares
In a study on AS flares, patients reported “the main perceived triggers of flare were stress and ‘overdoing it,’” Dr. Appleyard says. “Keep in mind ‘stress’ may mean both physical stress, such as an illness, or emotional stress. Excess fatigue may also trigger a flare.”
Unfortunately, beyond that experts don’t really know what causes AS to flare. “We really truly don’t understand all of the aspects of the inflammatory component,” Iversen says. “Environmental triggers are less clear than in [other inflammatory arthritis] for example, rheumatoid arthritis.”
How AS Flares Are Diagnosed
Doctors rely on individual patients’ experiences to determine if AS is flaring. “You should notify your doctor if your symptoms are out of the ordinary or more severe than your usual disease activity,” Dr. Appleyard says.
However, “there are objective ways to assess disease activity and functional ability in patients with AS, such as the BASDAI [Bath Ankylosing Spondylitis Disease Activity Index] and the BASFI [Bath Ankylosing Spondylitis Functional Index].”
These questionnaires measure the major symptoms of AS (fatigue, spinal pain, joint pain or swelling, inflammation of tendons and ligaments, morning stiffness) and the patient’s ability to cope with everyday life. “Rheumatologists use these measurements to help determine disease activity and to assess response to treatment,” Dr. Appleyard says.
In addition, AS “symptoms as a whole are related to increased levels of certain cytokines in the blood,” Dr. Appleyard says. Blood levels of these substances are closely correlated with the activity of the disease, she says.
You can use our ArthritisPower app to track your symptoms and disease activity and share your results with your doctor.
Treatment for Ankylosing Spondylitis Flares
Medications
“NSAIDs such as ibuprofen or naproxen help to address inflammation,” Dr. Appleyard says. “Occasionally steroid medications such as prednisone, which are potent anti-inflammatories, are used for severe flares not responding to more conservative measures.” NSAIDs are considered first-line therapy for people with ankylosing spondylitis; biologic drugs are typically recommended after people don’t get relief from taking NSAIDs.
If you find your AS flares are getting worse, lasting longer, or occurring more frequently, this could indicate you would be a good candidate for biologic medication or perhaps need to try a different kind of biologic medication to help prevent future flares from occurring.
Gentle exercise
“With ankylosing spondylitis, you actually feel better with exercise than you do with rest, so when patients begin to feel a flare coming on it’s really important to keep moving,” Iversen says. “You just need to do it in moderation and you need to really pay attention to the signals from your body.” Try tai chi, modified yoga, the elliptical machine, walking, range-of-motion exercises, even just stretching or deep breathing. Swimming and hydrotherapy are also well-tolerated, she says.
“I try to find a balance between rest and gentle exercise to keep my joints moving, even if all I can manage is some stretching while lying in bed,” Greatorex says. Short bits of exercise spread through the day are all that’s needed, Iversen says.
Heat or cold therapy
“Although there isn’t a lot of empirical data on the impact of ice or heat, many patients like warmth and some people really love cold — there’s no harm in using either heat or ice,” Iversen says. Dr. Appleyard suggests a heating pad or a hot bath or shower; in the morning, the warmth may help loosen up stiff joints.
Transcutaneous electrical nerve stimulation (TENS)
Although this sounds a little scary, Iversen says this device can be prescribed by your PT. “We call it an adjunct therapy that helps to modulate pain,” she says. TENS manages the pain of a flare by blocking the nerve signals to the brain. Although it hasn’t been scientifically proven to be effective, it’s safe as long as you are instructed on how to properly use it.
Tips on Coping with AS Flares
Prepare for a flare
When it comes to AS flares, an ounce of prevention is worth a pound of cure. Although you can’t actually stop a flare from striking, you can make sure to keep up with your exercise plan to better handle them. Strength training, aiming for proper posture, stretching, and endurance exercises for cardiovascular health will put you in better shape for when a flare strikes. Try these daily stretches for ankylosing spondylitis.
“I recommend my patients try to incorporate things that would promote spinal extension and rotation of the spine, and work on hip and knee strength,” Iversen says. You can work these techniques into your daily living. For example, take regular breaks from sitting at your computer, use a standing desk, and stretch out on your stomach propped on your elbows instead of sitting on the floor when playing with your kids, she suggests.
Develop your own pain management techniques
In addition to taking pain medication or steroids as needed, try employing mind/body techniques such as meditation to cope with AS pain. Certain exercises such as tai chi and even deep breathing (which helps promote chest expansion) also have benefits when it comes to the mental component. “Focusing on parts of your body that don’t feel pain and integrating breathing exercises into your meditation with maybe beach sounds or music will really help people to feel more relaxed and reduce the anxiety associated with having discomfort,” Iversen says.
Create time for rest in your routine
Is it important to know your limits and ask for help when you need it during a flare — or even before. “If I have warning and I can feel it coming on for a while beforehand, I slow down and take it easy,” Greatorex says. “Resting is a huge part of a flare for me. My husband takes over the housework, the shopping, driving where necessary.”
Manage stress and mental health
In addition to mind/body strategies for pain management, be sure to address other mental aspects of the disease. “Learn stress reduction techniques, and some patients find support groups helpful,” Dr. Appleyard says. Educating yourself about your disease and talking with your doctor ahead of time about what to do when you have a flare can help take away some of the unknowns.
When in the middle of an AS flare, Greatorex says, “the biggest thing though, as hard as it is, I remind myself that this too shall pass.”





