If you have rheumatoid arthritis or another kind of arthritis — chronic illneses with no cure — it’s highly likely you’ll spend an inordinate amount of time at your rheumatologist’s office. We’re talking about appointments every couple months, at a minimum, for years, decades, even indefinitely.
“I’ve been with my rheumatologist for 25 years,” says RA patient Lisa King. “When I first met him, I was in big trouble health-wise. He changed my life.”
I don’t like my rheumatologist — I lovemy rheumatologist. And I don’t say that lightly because historically, before my RA diagnosis, I wasn’t exactly a doctor lover. Some may even say I was hostile to the idea of going to the doctor. But now I love my guy for what I like to call the three Cs (full disclosure, I just made that up two seconds ago):
Chemistry: I have great convos about traveling and politics with my physician. I’m not the only one who digs their doc’s personality. “My rheumatologist wears funky boots and has a squishy phone cover,” says Victoria Wedge. “She’s fab!” Adds Victoria Bouabane, “my doctor was off sick last year for a while and I met up with his partner. I didn’t really click with him and I felt like just another patient.”
Competence: Seems obvious, but your doctor has to know what the heck they’re doing. Adds Barbara Mendez: “My rheumatologist is very knowledgeable and uses her common sense along with her book-smarts.”
Comfort level: This is perhaps the most important criterion, notes Ashira D. Blazer, MD, instructor of medicine in the division of rheumatology at NYU Langone Medical Center in New York City. I talk to my RA doctor, Dr. Feldman, about everything — arthritis pain, of course, but also diarrhea, menopause, disgusting nose bleeds, and being transgender. Nothing about my health or life is sacred or off-limits because everything is relevant.
“You have to feel comfortable with your doctor,” Dr. Blazer explains. “You have to feel safe talking about what’s bothering you and if you’re comfortable taking your medication. You have to trust your doctor to come up with a therapeutic plan to help you feel better.”
Admittedly, not everyone has a big pool of rheumatologists to dip into, especially patients in less populated areas. Many have to travel hours just to find a doctor in a 100-mile radius. But if you have the luxury of choice, be picky. This is your health, your life, and your future at stake.
“Make sure you have a good relationship with your doctor,” insists Dr. Blazer. “If you don’t have that comfort level, perhaps keep looking around.”
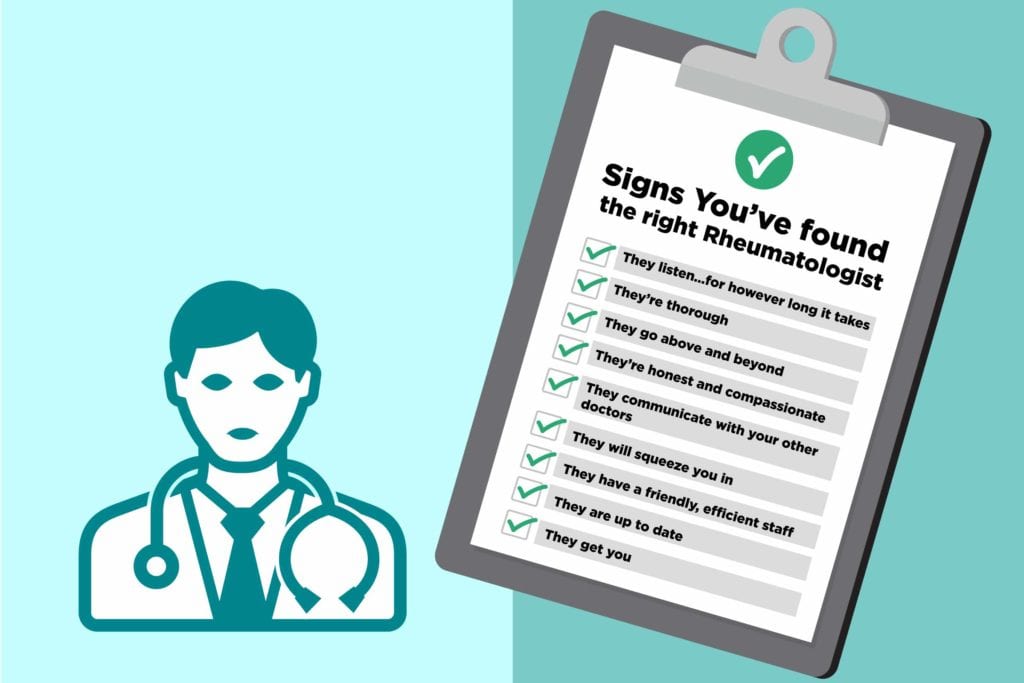
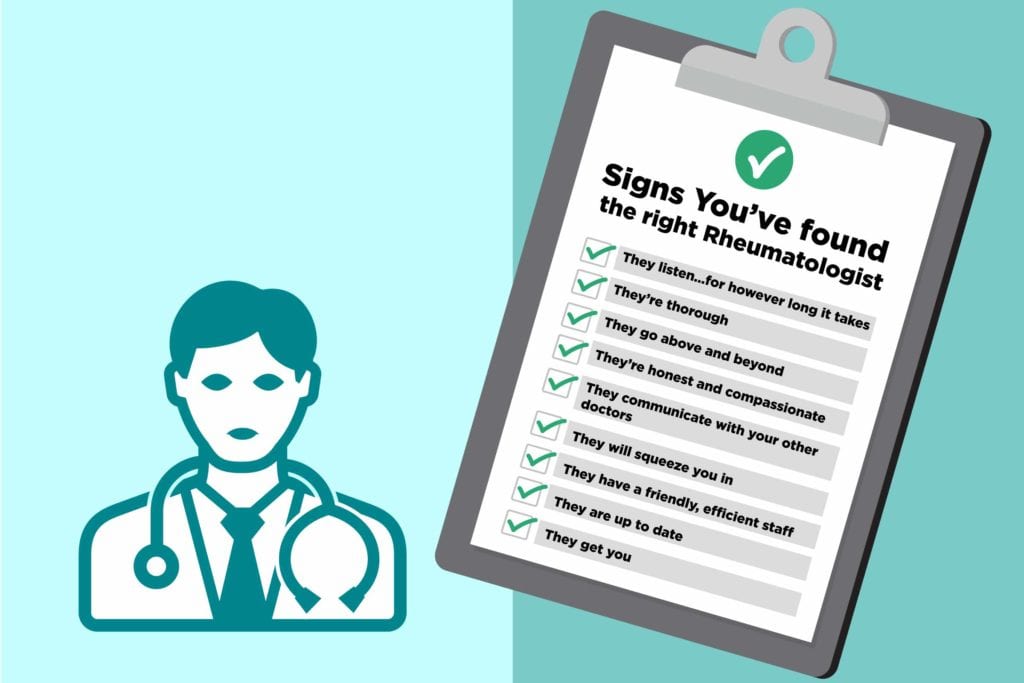
Signs You’ve Found the Right Rheumatologist
1. They listen — for however long it takes
Many patients feel rushed in and out of the office, leaving them wondering if their doctors even heard anything they said. A good rheumatologist will let you talk about every ache and pain, plus the weather (which could be the reason for your pain!). “Mine listens and doesn’t rush me,” says Becki Barnhill.
A specialist like this shouldn’t spend two minutes with you. “It’s important to spend time with and educate the patient,” says Dr. Blazer. “If you don’t understand what’s going on, you’re not going to take care of yourself appropriately.”
2. They’re thorough
Since a lot of patients get shy or forgetful once they step foot in the doctor’s office, Dr. Blazer recommends bringing a list of concerns and questions to go over with your doctor. If she’s cool going over that list, that’s a good sign. She should also have no problem explaining your lab tests and bloodwork in detail. You should leave your rheumatologist appointment feeling like no stone was left unturned.
“My rheumatologist takes his time, explains his thought process, and why he is doing what he is doing,” says Deb Hanzelik. Barbara Mendez appreciates that her doctor “talks ‘to’ me, not ‘at’ me.”
3. They go above and beyond
Don’t you just hate it when you have to call your doctor’s office to get test results? It’s a nice touch when they take the time to reach out to you first. One of my RA pals says her doctor actually calls her on weekends. My doctor called me the day aftermy last appointment to talk about my thyroid test results. I was kind of shocked at his expediency but I greatly appreciated it. Mendez is grateful for that kind of care, too: “My doctor will call when my inflammation markers are elevated,” she says, “to see if I want to come in sooner to see her or just start a prednisone burst pack.”
New technology may mean new norms and ways of communicating for a lot of rheumatologists and their patients. “I have my doctor’s personal cell phone number so if I never need anything, I can call or text her and she always gets back to me right away,” says Layla Tzoras.
And yet Hanzelik’s rheumatologist still takes the time to write her by snail mail. “I received a letter from him four days after my second appointment,” she recalls. “In it, he stated that he was giving my case more thought and added in new tests and sent me ‘scripts to get them done. Can’t ever say I had a doctor think more on my case after I left the office. He has called me after hours on his personal cell phone to review blood results when he could have easily left me a message to call him the following day.”
4. They’re honest and compassionate
When you’re managing a chronic disease, you don’t always get good news. So a doctor’s bedside manner matters. A lot. “He treats me like an adult,” Murray Mu says about his rheumatologist. “He’s perfectly frank and at the same time he shows a lot of empathy.”
Odds are that your doctor will not have arthritis, so they probably will not know what it literally feels like to live with a chronic inflammatory disease, says Dr. Blazer. Though Robin Martinez’s RA doctor has chronic back pain and her nurse practitioner has RA, and she feels like that has a positive impact on her treatment. “He understands the pain component,” she says. “And my nurse has been on many of the RA meds and is now on biologics.”
However, there are many ways your doctors and nurses can show they are able to sympathize with you, and that includes doing everything they can to make sure you have as little pain as possible. If you have a doctor who will stop at nothing to make you feel better, you’ve got the right guy or gal. There should always be another avenue to go down. Failure should not be an option.
5. They communicate with your other doctors
Inflammatory arthritis can cause or be associated with a host of ancillary issues — eye problems to anxiety and depression to other autoimmune diseases. So it’s essential that your rheumatologist be in contact with all of your doctors, especially your primary care physician. “Your primary should be looped in,” Dr. Blazer says, “because they’re responsible for your holistic care. They should be aware of what’s going on. Continuity of care is essential.”
Debra DeWitt’s rheumatologist keeps track of the tests her other doctors order and “she discusses those results with me, too. She lays out options, then helps me decide what to do.” Mendez appreciates that by the time she comes in the room, her doctor has already read and gone through all of her recent doctor appointments and their notes and lab results/tests. It’s not like Evelyn Wood speed reading right in front of her (that’s a joke for Gen-Xers).
6. They will squeeze you in
If you’ve been in the military, you know it can take eons to get an appointment at a veteran’s hospital and there’s not much you can do about it. But for the rest of us, it’s totally unacceptable to wait months for an appointment, especially if you’re in excruciating pain. A good rheumatologist’s office will find time for you.
Vanessa Gonzalez couldn’t get an appointment with her doctor for two months and resorted to popping a lot of ibuprofen, which could be dangerous to her kidneys. “The receptionist told me there were no openings,” she laments. “If I didn’t at least take ibuprofen, I wouldn’t be able to go to work anymore, let alone get up to make myself something to eat. I was so irritated with my doc.”
7. They have a friendly, efficient staff
The receptionist, the nurses, the lab technicians, and everyone in your rheumatologist’s office will feel like family after you’ve seeing them for years. (Hopefully, it’s not a dysfunctional family.) The staff at my doctor’s office helps make my visits as pleasant as possible. I look forward to seeing Magda at the reception desk; she always makes sure I have enough parking validation. Selma draws blood out of my thin-skinned hand like such a pro that it doesn’t even hurt anymore. And Arliz always gets me a pillow for my throbbing feet while I get my three-hour infusion. They run the office like a well-oiled machine.
“I do love that my nurse knows me by name,” Shannon Lockheart agrees. “She draws my blood painlessly every time and she always calls me back with whatever answer I need after consulting with my rheumy.”
8. They are up to date
How do you know if your doctor is aware of the most recent advances in RA treatment? “All doctors are required to keep up with continuing medical education, the latest literature, and the newest drugs,” says Dr. Blazer, though she adds that physicians affiliated with academic medical centers tend to have more rigorous standards for continuing education. “I like that my doctor is up on all things current,” says DeWitt.
When choosing a rheumatologist, you can search online to see if your doctor attends or speaks at conferences or publishes research in medical journals. Also check if their group, practice, or university lists specific requirements for making continuing education a part of their mission as a physician, Dr. Blazer suggests. You can also call the office and ask what is expected of their doctors. (I wouldn’t, but you can! Just being honest.)
9. They get you
According to an article in the Harvard Business Review, sharing a cultural or racial background with your physician can “help promote communication and trust.” Since 58 percent of doctors are white and, according to a UCLA study, only 9 percent of academic medical practices have procedures for connecting patients to LGBTQ-competent physicians, it can be difficult for minorities and gay folks to find doctors they feel the most comfortable with.
Not saying that you should only see doctors who are exactly like you, but it could help. Unfortunately it’s nearly impossible. I can’t even find a stat that says how many LGBTQ doctors there are. But I did find a stat that says 30 percent of sexual minority medical students remain in the closet for fear of discrimination.
However, this brings me back to points one and four. Even if your doctor has a different background from you, being compassionate and a good listener can go a long way.


Signs You Need to See a Different Rheumatologist
1. They minimize your pain
Especially if you’re a woman. Research shows that 70 percent of people with chronic pain are female, and yet there can be a real disparity in how they are treated. Research indicates women’s pain is more likely to be ascribed to emotional rather than physical causes. When men and women present with similar symptoms, women are more likely to be prescribed sedatives over pain medication.
The gender bias is real but you really don’t have to deal with it. If you feel like your rheumatologist (or any doctor) isn’t taking your pain or other symptoms seriously, move on to someone who will. “It’s definitely true that women feel less heard in the doctor’s office,” Dr. Blazer confirms.
2. They treat the symptom, not the patient
You’re not a guinea pig; you’re a human being, so you shouldn’t be treated like a faceless cadaver by your rheumatologist. Stacy Nystrom experienced this at her last appointment. “I’ve been talking Plaquenil for a little over a year, and my dose increased a few months ago, which has helped,” she explains. “But I have a new insurance plan for 2019 and now it’s costing me almost $100 per month. My rheumatologist’s recommendation? ‘If you can’t afford it, stop taking it.’ What? That’s all you can come up with? I was so irritated and anxious.” Thank you, next.
3. They obsess about your weight
“Have you ever considered going on a diet?” That question is not the answer to every problem an arthritis patient has. And yet, many of us find ourselves having that conversation with our doctors more than we’d like. Weight management is a real issue for rheumatoid arthritis patients because we are more likely to develop diabetes and heart disease. “There is an obesity epidemic and it does affect inflammatory arthritis. Every pound you’re overweight puts four pounds of added pressure on your knees,” Dr. Blazer says. “TNF inhibitors like Humira and Enbrel don’t work as well in people who carry excess weight.”
At the same time, she acknowledges that every conversation should not revolve around weight management. “It can be a delicate subject,” she adds. “But it is important to be able to talk about healthy living and nutrition and weight management. That said, it should be ‘a part of.’ It shouldn’t feel like a badgering session.”
4. You see a PA more often than the rheumatologist
It’s been shown that physician assistants are “actually better and more efficient than physicians at following protocol procedures like checking blood sugar or blood pressure,” Dr. Blazer says. “But for complex medical diseases like rheumatoid arthritis, physicians have more training.”
Make sure you understand how your practice uses physicians versus other care providers such as physician’s assistants or nurses. It’s perfectly fine to have different kinds of providers on your health care team, but you should know in what circumstances you will tend to see which experts. When you’re chronically ill, you want to feel like you’re getting the absolute best care possible.
5. The staff seems like a disaster
“It is impossible to get anyone on the phone at my rheumatologist’s office,” says Michelle Montcalm. “Every time I call, it goes straight to voice mail. Often, my calls are not returned or at best, the receptionist calls back two to three days later. Very frustrating!” If you always get the runaround on the phone, experience long waits to see the doctor, and get overall major ’tude, find a new practice. This is your health. You can’t afford to mess around with that!
Keep Reading
- 17 Things Your Rheumatologist Wishes You’d Stop Doing Already
- 15 Things Doctors Don’t Always Tell You About Rheumatoid Arthritis (But You Really Should Know)
- News: A Rheumatologist Shortage Is Looming





