On average, it can take nearly six years for a person to get diagnosed with lupus, according to the Lupus Foundation of America. Why so long? “Lupus can present in so many different ways,” says Ashira Blazer, MD, a rheumatologist and assistant professor in the department of medicine at NYU Langone Health in New York City. The many different symptoms of lupus can cause it to take a long time for patients themselves to suspect they could have lupus or a related immune system condition, send patients to different kind of providers depending on which symptoms they experience, and can lead to misdiagnoses of other conditions besides lupus.
Lupus is an autoimmune disorder in which the immune system begins to attack the tissues in just about every organ in your body, causing widespread, chronic inflammation.
But with lupus, what sends you to the doctor’s office, at least at first, can be a range of symptoms that seem vague and non-specific.
“The symptoms that patients most complain about are the symptoms that they can outwardly feel and see. They’re going to say ‘I feel really tired. I’ve been losing weight, my joints kind of hurt. What’s this weird rash?’” Dr. Blazer explains.
These symptoms can be mistaken for other conditions. Sometimes a lupus rash can look like rosacea. Fatigue can be a sign of a thyroid disorder, diabetes, or a host of other health problems. “So often lupus patients end up misdiagnosed for extended periods of time until someone can put it all together,” Dr. Blazer explains.
And that’s a problem since the longer it takes to get diagnosed with lupus, the longer treatment is delayed — and the more the disease can damage your body, especially your kidneys. To prevent this from happening to you, here are the things you need to know and ask for to get the right diagnosis if you have any suspicions you could have lupus.
What to Expect At the Doctor’s Office
Patients with lupus tend to see different specialists, depending on what part of the body is affected at first, notes Michelle Petri, MD, a rheumatologist and director of the Lupus Center at Johns Hopkins Medicine in Baltimore, Maryland. “So if they’re presenting with skin rash, they may go to a dermatologist first. If they’re presenting with those non-specific symptoms like fatigue, anemia, and some hair loss, they might go to a primary care doctor or an internist first.”
After taking a thorough medical history, the doctor may be able to piece the clues together, especially if:
- You’re a young woman — 90 percent of all lupus patients are women, and typically they’re between the ages of 15 and 44, according to the Lupus Foundation.
- You’re African American or another woman of color, like Latina, Asian, or Native American, who have higher rates of lupus.
- Your rash gets worse after you’ve been out in the sun.
- You have joint pain and swelling, especially in the morning.
That’s when your doctor may refer you to a rheumatologist, who should manage your care going forward if you are diagnosed with lupus.
“Rheumatologists don’t do it alone,” says Dr. Petri. “If a person has a renal lupus [lupus that affects the kidneys], I will refer the patient to one of our nephrologists for a kidney biopsy. And if they have a rash and my initial attempts at controlling it are not successful, I will very likely ask for help from a dermatologist. But in both cases the patient will return to me.”
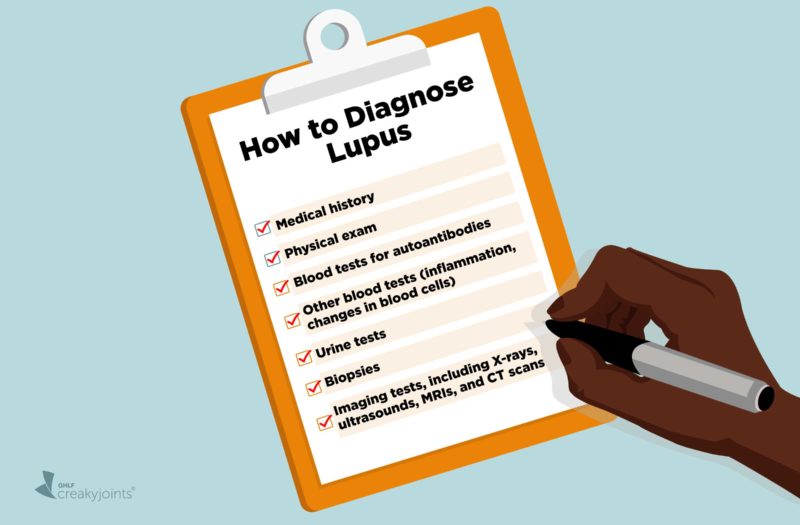
Keep in mind that that there is no single test that can diagnose lupus. Confirming a lupus diagnosis depends on the combined results and interpretation of many different factors, including:
- Medical history
- Physical exam
- Blood tests for autoantibodies
- Other blood tests (for inflammation, changes in blood cells, and more)
- Urine tests
- Biopsies
- Imaging tests, including X-rays, ultrasounds, MRIs, and CT scans
Taking a Medical History and Physical Exam
Doctors are often looking for two things as they do a physical exam and take your medical history: whether the disease is systemic (all over) and is causing inflammation.
“Lupus is a disease of dysfunctional white blood cells. Anywhere the blood can go, lupus can go, so a doctor should be thinking about a disease that affects multiple parts of the body,” says Dr. Blazer. Some of the organs that are most commonly affected are the skin and the kidneys. Even your nervous system can be affected, which is why lupus patients can experience memory loss or seizures.
“The other thing doctors should be looking for are symptoms of immune activation,” she says. Besides looking for fevers and weight loss, doctors are looking for joint damage and arthritis. “When you find that someone has pain, swelling, and stiffness that is worse than the morning time, especially when it lasts more than 30 minutes, you start thinking that this might be caused by an autoimmune condition,” Dr. Blazer explains.
Skin rashes are another common symptom, especially the “butterfly” or malar rash that can appear on your cheekbones, the bridge of your nose, and along your jaw (including your chin).
Using Diagnostic Criteria Developed for Lupus
To help narrow the diagnosis, doctors often rely on a set of criteria developed by the American College of Rheumatology or from the Systemic Lupus Erythematosus International Collaborating Clinics Group (SLICC).
To meet the criteria, “a total of four things needed to happen to the patient, but at least one of those four must be a clinical manifestation [a symptom], and at least one of the four must be an autoantibody. It isn’t enough just to have clinical things. And it isn’t enough just to have lots of lupus antibodies. There has to be some of both,” Dr. Petri explains.
Some examples of symptoms that qualify as clinical manifestations and can signal that the organs are involved include:
Skin rashes
Besides the “butterfly” rash, there are other types of rashes that affect the skin in lupus, including a discoid rash. “It can occur on the scalp, in the ears, on the face, on the forearms. It’s hard to treat and often at the very beginning there’s already permanent scarring. If it happens on the scalp, the hair loss is permanent. If it happens on the face, it heals with hypo or hyperpigmentation,” says Dr. Petri.
Chest pains
This can indicate that there is fluid around your lungs or pericarditis, which is inflammation of the heart.
Swelling in your legs or puffiness around the eyes
This may signal your kidneys aren’t working properly.
Memory loss, seizures, numbness or tingling
These indicate neurological changes.
Arthritis
Doctors look for signs of joint swelling, pain, and stiffness.
Antibody Tests to Diagnose Lupus
Besides the physical exam, doctors will also run blood tests to look for autoantibodies in your blood, which is a sign that that your immune system is attacking itself. “A lot of times primary care doctors will do an ANA test, which is an anti-nuclear antibody protein that certain kinds of white blood cells make when targeting your body,” Dr. Blazer explains.
Most people who have lupus will have a positive ANA test, so if the test is negative, that’s a good sign your symptoms are due to something other than lupus. But just because you have a positive ANA test doesn’t automatically mean you have lupus. Many things can cause a positive ANA,” says Dr. Blazer. “This antibody is more common in people who are older. It is more common in women. It is more common in people who have family members who have an autoimmune disease.”
Still, a positive ANA can suggest you have lupus, which is why rheumatologists will then look for other antibodies, including anti-dsDNA, anti-SSA/RO, and anti-Smith, which are more specific to lupus. And about 50 percent of patients have something called antiphospholipid antibodies, says Dr. Petri.
A physical exam for lupus symptoms and antibody tests are not usually enough to clinch a lupus diagnosis. Doctors will usually perform some of these additional tests to further confirm lupus and rule out other similar diseases.
Other Tests to Diagnose Lupus
- Complete blood count, to see if you have low white blood or platelet counts (both signs of lupus) or hemolytic anemia, which when the red blood cells break apart because of inflammation
- Urine test to check for protein, a sign that your kidneys have been affected
- Blood tests for inflammatory markers erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP)
- Blood tests for activity of the complement system, which are proteins that are part of the immune system (low levels of complement proteins C3 and C4 can indicate lupus)
Biopsies
- Of your kidneys if you had protein in your urine. “A kidney biopsy tells us how long the kidney injury has been going on. Did it just start or has it been there a really long time and there’s scarring? There are five different classes of lupus kidney injury. Being able to diagnose which class the patient has can dictate how we’ll treat them,” says Dr. Blazer.
- Of rashes, especially the discoid rash or subcutaneous rash, which have distinctive signs.
Imaging tests
- X-rays to check for deformed joints (that aren’t noticeable during a physical exam) or damaged ones. Chest x-rays can also show fluid buildup in the lungs.
- Ultrasounds of the joints, to check for inflammation in the fluid-filled sheaths surrounding the tendons or in the connective tissues; or of the kidneys
- Echocardiogram (ultrasound of the heart) to see how well the heart is functioning
- CT scans, to check for pancreatitis, in case you have pain or vomiting; or the GI tract (abdominal pain)
- MRIs to check for problems in the nerves, spine, or brain in case you are feeling numbness, tingling, or weakness
You likely will not need all of these tests. But you should absolutely insist on a thorough physical exam and lab tests to look for autoantibodies to see whether you have lupus or another autoimmune disease.
Chances are, if you’re seeing a rheumatologist because you have concerns about having lupus, you’ve already seen quite a few different doctors or health care providers by now. We know this process can be exhausting and exasperating. We are here for you to help make things easier.
Become part of the CreakyJoints community (you can sign up in the upper right corner of our site) and follow us on Facebook, Twitter, and Instagram for ongoing support and education.
Here are more of our educational resources on lupus, which are updated regularly, or connect with some of our great partners in this community. Check out #LupusChat on Twitter for ongoing conversation and support among people living with lupus. We also recommend checking out the programs from our fellow non-profit patient advocacy community, Lupus and Allied Diseases Association.
Get Involved in Lupus Research
If you are diagnosed with lupus or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
Keep Reading
Clinical manifestations and diagnosis of systemic lupus erythematosus in adults. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-systemic-lupus-erythematosus-in-adults.
Diagnosing and Treating Lupus. Centers for Disease Control and Prevention. https://www.cdc.gov/lupus/basics/diagnosing.htm.
Diagnosing lupus. Lupus Foundation of America. https://www.lupus.org/resources/diagnosing-lupus-guide.
Diagnosing Systemic Lupus Erythematosus. NYU Langone Health. https://nyulangone.org/conditions/systemic-lupus-erythematosus-in-adults/diagnosis.
How is lupus diagnosed? Johns Hopkins Lupus Center. https://www.hopkinslupus.org/lupus-info/diagnosing-lupus.
Interview with Ashira Blazer, MD, a rheumatologist and assistant professor in the department of medicine at NYU Langone Health in New York City
Interview with Michelle Petri, MD, a rheumatologist and director of the Lupus Center at Johns Hopkins Medicine in Baltimore, Maryland
Lockshin M. Dealing with Uncertainty in Your Lupus Diagnosis. Hospital for Special Surgery. https://www.hss.edu/conditions_dealing-with-uncertainty-lupus-diagnosis.asp.
Lupus. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Lupus.
Lupus. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/lupus/diagnosis-treatment/drc-20365790.
Lupus facts and statistics. Lupus Foundation of America. https://www.lupus.org/resources/lupus-facts-and-statistics.