

If you’re living with arthritis, chances are you’ve thought about trying to eat a more anti-inflammatory diet. Or perhaps friends, family, or even your doctor has suggested it to you. After all, systemic inflammation is a root cause of autoimmune arthritis like rheumatoid arthritis and it also can exacerbate joint wear-and-tear in osteoarthritis.
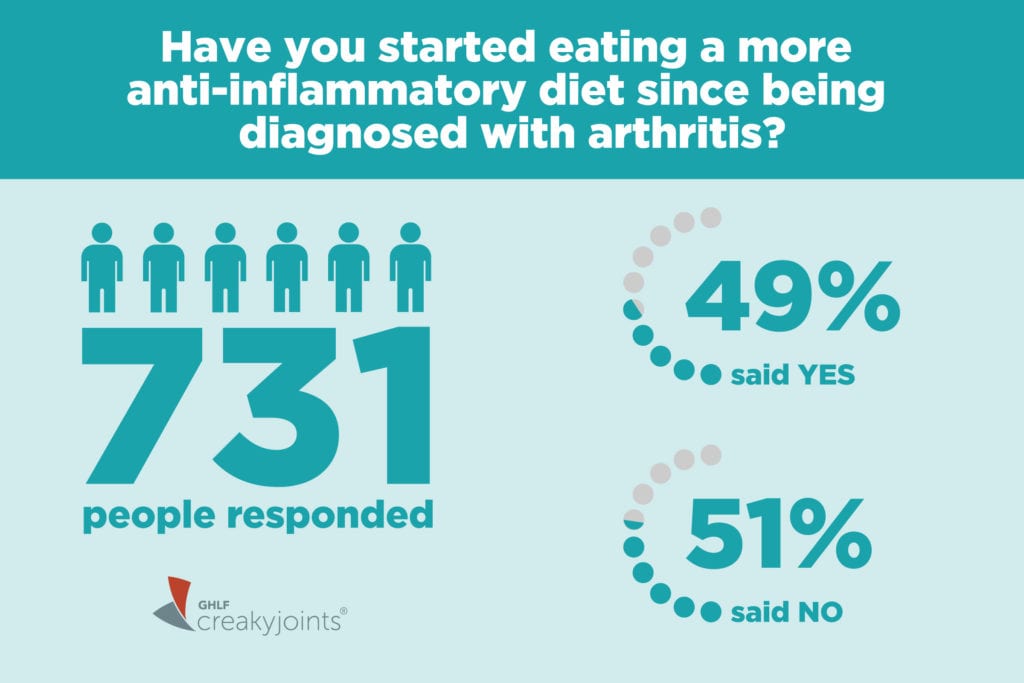
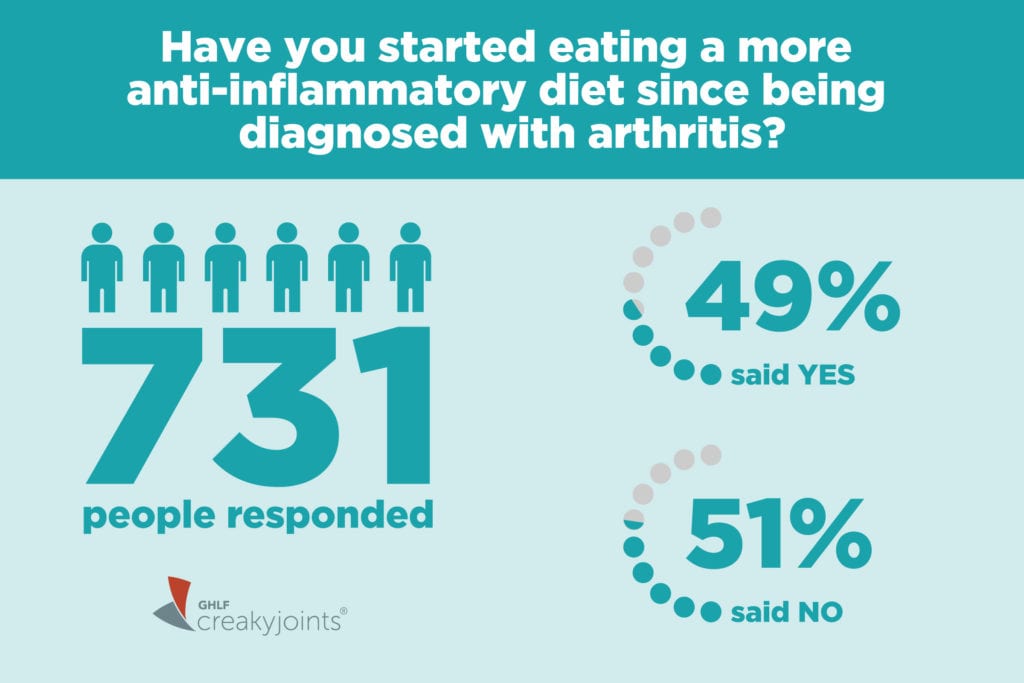
In a recent ArthritisPower Community Poll, we asked people whether they’ve started eating a more anti-inflammatory diet since being diagnosed with arthritis. Out of 731 respondents, about half said that they have started eating a more anti-inflammatory diet since being diagnosed with arthritis.
Some respondents may have they felt they already were eating an anti-inflammatory diet to begin with, so they answered, “no.” Others may not know exactly what constitutes an anti-inflammatory diet.
But for those considering eating a more anti-inflammatory diet, exactly what to include or avoid is far from a black-and-white answer.
The Truth About Anti-Inflammatory Diets for Arthritis
While there is some research that shows a connection between diet and inflammation, researchers are still trying to understand the link between specific foods and arthritis symptoms.
For example, researchers from Brigham and Women’s Hospital and Harvard Medical School found that young and middle-aged women with an inflammatory diet pattern had a greater risk of developing rheumatoid arthritis than those with a less inflammatory diet pattern — but the link may have to do more with weight than with specific food choices.
The results were less strong after researchers accounted for the participants’ body mass index (BMI). Having excess body weight is also inflammatory, so if people who are overweight also eat more inflammatory foods, it’s unclear which is having more of an impact.
Most doctors would happily encourage their arthritis patients to follow a Mediterranean-style diet since research has linked it to a lower risk of type 2 diabetes and heart disease and an increase in longevity. This style of eating means consuming mostly plant-based foods, such as fruits and vegetables, whole grains, legumes, and nuts; replacing butter with healthy fats such as olive oil; and limiting consumption of beef or other red meat to once or twice a month.
What’s less clear: whether there are any significant benefits to following diets that are more restrictive or specialized than the Mediterranean diet. Some people contend these plans may help heal the immune system and fight inflammation, but good scientific research is lacking.
The fact is, there’s a lot about the personalization of diets — why certain foods might be especially beneficial or harmful in certain people — that researchers just don’t have answers to yet.
If you’re thinking about making a significant change in your eating pattern to help manage your arthritis symptoms, make sure you talk to your doctor about it. You might unnecessarily eliminate foods you love or put yourself at risk for certain nutrient deficiencies. It’s critical to incorporate any diet changes into an overall treatment plan — and not consider them as a replacement for medications your doctor prescribes to treat your disease.
Easy Ways to Make Your Diet More Anti-Inflammatory
1. Cook more meals at home
One thing that anti-inflammatory diets all have in common: To follow them well, you have to cook your own foods at home, according to James D. Lewis, MD, a professor of medicine and epidemiology at the University of Pennsylvania and a researcher of the role of diet in inflammatory bowel disease. During a recent ArthritisPower webinar, Dr. Lewis highlighted the fact that scientists suspect that additives in our food may contribute to inflammation.
When you buy fresh ingredients and make meals at home yourself, rather than eat takeout or processed prepared meals, you reduce your exposure to such chemicals. You’re also less likely to consume extra sugar and fat, which add calories and could affect weight gain. Keep in mind that even nutritious-sounding products (such as gluten-free snacks) in the “health food” aisle at your grocery store can be highly processed and packed with additives.
2. Don’t drink soda or sugar-sweetened beverages
Sugar is a pro-inflammatory ingredient with little nutritional value. Eating natural sugars found in fruit or dairy is perfectly fine — have you ever heard of someone gaining weight from eating too many strawberries? — but sugar that’s added to foods like cereal, salad dressing, and frozen foods isn’t doing your body any favors. Sugar in the liquid form of soda, juice, and energy drinks is especially problematic because some research suggests that our bodies don’t register liquid calories the same way as the ones we have to chew. Cutting out soda, sugar-sweetened beverages, and sugar from treats like dessert is one of the best things you can do to make your diet less inflammatory and more arthritis-friendly.
3. Eat a fruit or veggie at every meal
Certain restrictive anti-inflammatory diets can drive you crazy remembering which specific vegetables or fruits are off-limits for various reasons. But most Americans are simply eating far too less produce in general. Eating more produce supplies your body with filling fiber and a wide range of disease-fighting plant compounds called phytonutrients—it also helps crowd out less healthy options from your plate, like processed carbs in the form of chips, pretzels, and sweets. According to 2017 CDC data, only 10 percent of Americans meet the recommendations of 1.5 to two cups of fruit and two to three cups of vegetables a day.
Instead of focusing on avoiding certain fruits or veggies, focus on making sure you eat a serving of produce every time you nosh. Top your breakfast yogurt or oatmeal with berries. Have carrots or peppers and hummus as a mid-morning snack. Have a salad at lunch. Eat an apple and peanut butter for an afternoon snack. Always have a side of veggies, like roasted broccoli or steamed spinach, with dinner.
Keep Reading
- 8 Anti-Inflammatory Foods for Arthritis Nutritionists Want You to Eat More Often
- Weight Loss Tips that Can Specifically Help If You Have Arthriti
- The Keto Diet and Gout: Myths and Facts
Learn More About ArthritisPower
This question was one of our monthly ArthritisPower Community Questions, offering ArthritisPower participants an opportunity to learn from each other and provide our research team insights.
If you’re diagnosed with RA or a musculoskeletal condition, participate in future polls like this, as well as research studies, by joining CreakyJoints’ patient research registry, ArthritisPower. As a patient-led, patient-centered initiative, our research team is committed to investigating research topics that matter most to you.





