Ask anyone on the street how they slept last night and more likely than not, they’ll complain about going to bed too late, waking up too early, or tossing and turning for one reason or another. Americans are notorious for skimping on sleep: National data from the Centers for Disease Control and Prevention show that more than one-third of adults are not getting enough sleep on a regular basis.
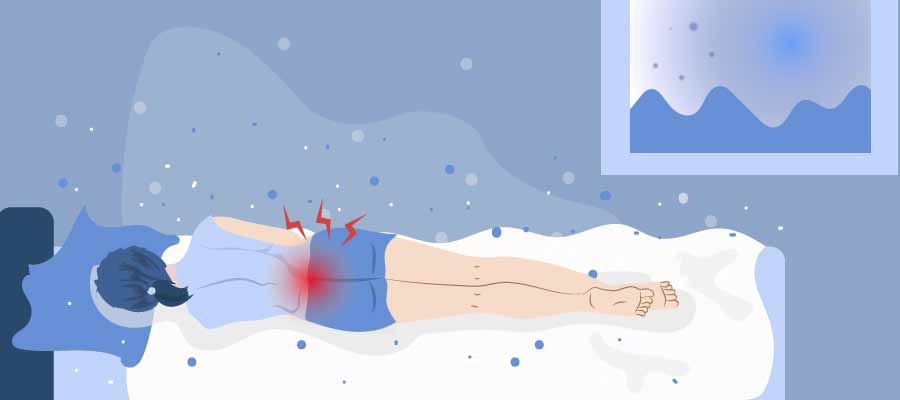
But for people with arthritis or other musculoskeletal or rheumatic diseases, poor sleep can be a devastating side effect. Pain and inflammation from the disease directly impact the ability to get a restful night’s sleep.
It’s no wonder that when we asked members of CreakyJoints and ArthritisPower, our patient-powered research registry, in a recent Community Poll if they wish they slept better each night, a resounding 95 percent of 1,886 respondents said yes. (You can use our ArthritisPower app to track your symptoms and disease activity and share your results with your doctor.)


Pain, Inflammation, and Sleep: A Vicious Cycle
Pain and inflammation from systemic inflammatory diseases like rheumatoid arthritis, lupus, or ankylosing spondylitis directly impact sleep quality. Research shows that people with osteoarthritis also experience sleep problems related to joint pain and immobility.
“There’s an association between inflammatory cytokines [immune system proteins] and sleep quality,” says rheumatologist Shraddha Jatwani, MD, adjunct clinical assistant professor of medicine at the Indiana University School of Medicine. While the exact nature of the link between sleep and pain is still an active area of research, it is bidirectional — too little sleep makes pain feel worse and pain negatively affects sleep.
Not getting enough sleep is linked with a laundry list of other health problems, including many that arthritis patients are already prone to, such as depression and heart disease.
The Link Between Sleep Disorders and Arthritis
Sleep disorders, such as obstructive sleep apnea, restless leg syndrome, and insomnia, also play a key role in the sleep quality of people with arthritis and rheumatic diseases.
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea is a condition in which your breathing repeatedly stops and starts throughout the night. It occurs when your airway becomes blocked while you sleep. In most cases, patients aren’t even aware this is happening. Their main clues are very loud snoring and waking up feeling tired despite thinking they got enough sleep.
OSA increases your risk of autoimmune disease and vice versa, says Dr. Jatwani. Research shows sleep apnea is more common among people with rheumatoid arthritis and gout, for example.
In addition to making you sleep poorly and wake up feeling unrested, untreated sleep apnea can raise your risk for high blood pressure, heart disease, stroke, and other serious complications. It’s important to talk to your doctor about seeing a sleep specialist if you suspect you could have sleep apnea (more on this below).
Restless Leg Syndrome (RLS)
Restless leg syndrome is a condition that causes uncontrollable urges to move your legs, often because you’re experiencing an uncomfortable sensation. Studies indicate that restless leg syndrome is more common among people with rheumatoid arthritis and lupus.
Insomnia
A classic definition of insomnia is difficulty falling sleep or staying asleep throughout the night. While common in nearly all kinds of arthritis and related diseases, insomnia can manifest differently in various diseases. In RA, for example, people who are having active flares tend to take longer to fall asleep (known as sleep latency), says Dr. Jatwani. In people with ankylosing spondylitis or axial spondyloathritis, waking up in the second half of the night in pain — sometimes so bad that people need to get out of bed to walk around — is common.
How a Rheumatologist Helps Patients Sleep Better
For her part, Dr. Jatwani always asks patients about their sleep during checkups. But if your doctor doesn’t ask and you find yourself sleeping poorly, bring it up.
“Sleep disorders can limit patients’ subjective improvement of how they’re doing,” she explains. That means even if your bloodwork, imaging, and physical exam reveal that your treatment is working to reduce disease activity, “patients who don’t sleep well could perceive themselves not feeling better.”
It may not be realistic to achieve a so-called perfect night’s sleep if you have chronic pain, but there’s always room for improvement and adjustments to try.
Increasing your sleep quality is critical to your disease management and overall health. Check out the following tips Dr. Jatwani discusses with her own patients.
1. Start with sleep hygiene basics. According to the National Sleep Foundation, sleep hygiene “is a variety of different practices and habits that are necessary to have good nighttime sleep quality and full daytime alertness.” For many people, sleep hygiene is basic common sense:
- Don’t eat food (especially large, heavy, high-fat meals) close to bedtime
- Don’t consume alcohol or caffeine close to bedtime
- Don’t use electronics (TV, phone, tablet) close to bedtime
- Keep your bedroom dark and cool
- Use your bed for sleep and sex only
But even though we know we should be following the advice on this list, the reality is that many habits (like social media scrolling or late-night snacking) are tough to break. Take a hard look and try to cut out the habits that might be affecting your sleep quality. Dr. Jatwani says that avoiding caffeine in the afternoon and evening has a particularly important impact on many of her patients.
2. Ask about seeing a sleep specialist. Sleep disorders are complicated and often can’t be treated by your primary care doctor or rheumatologist. Even insomnia “has so many nuances that could be better addressed by a sleep physician,” says Dr. Jatwani. If you’re experiencing the following signs of a sleep disorder, ask about a referral to a sleep specialist.
- Snoring at night
- Waking up tired
- Daytime sleepiness
- Fatigue even after getting 8 hours of sleep (that seems different than the fatigue you typically experience from your inflammatory disorder)
If you do get diagnosed and start treatment for, say, obstructive sleep apnea, it can have a big impact on improving your sleep quality.
3. Re-examine your medication routine with your doctor. Medications you take to treat your arthritis can have a direct or indirect impact on sleep. If you’re experiencing sleep problems, consider how your medication could be playing a role and talk to your doctor about it. Alternative drugs or a different dosing schedule could help minimize the impact on your sleep.
- Prednisone or other corticosteroids are sometimes given as a split dose, which means you take one pill in the morning and one at night. For some people, the nighttime dose can cause insomnia. Your doctor may recommend avoiding split dosing or suggest that you take the nighttime dose earlier in the evening instead of right before bed.
- Methotrexate and some other medications can cause nausea as a side effect. “We often tell people to take them at bedtime so they can sleep through and avoid nausea,” says Dr. Jatwani. “But if that’s affecting your sleep, ask about taking it earlier in the day or with some food.”
It’s also critically important to follow your treatment plan and take your medications as prescribed, because “once patients’ disease is better controlled, it improves sleep,” says Dr. Jatwani.
The key, she says, to give it time. “DMARD medications can take four to six weeks to start working, so this is counseling we have to do with patients. Try to be patient, work with us. Let’s get your disease under control and that will help your sleep quality.”
4. Consider physical activity part of your treatment. In addition to sleep hygiene, another practical tip Dr. Jatwani shares with patients is the importance of regular physical activity, such as yoga or gentle cardio such as walking or swimming. “Exercise improves quality of life and sleep quality. Exercise helps decrease overall inflammation in the body, which may help improve sleep.” She says that starting physical therapy or exercise routines has helped many of her patients feel and sleep better.
5. If you feel sad, hopeless, anxious, or just not yourself emotionally, tell your doctor. Depression and anxiety are common in people with chronic pain and they also seem to play a critical role in the relationship between pain and sleep. Depression or anxiety increases the odds that you will experience poor sleep (and more pain as a result). You might not think your rheumatologist or primary care doctor can help you with mental health issues, but you need to let your doctor know. Watch this video about the importance of caring for your mental health with arthritis.
Here are general health and mental health resources for your reference:
- To find local support groups and services, you can call 1-800-950-NAMI (6264) or email info@nami.org. The NAMI HelpLine can be reached Monday through Friday, 10 AM to 6 PM, EST.
- For a counselor or therapist in your area, view the resources page at Mental Health America.
- If your mental health concern is an emergency for you or someone else, you should call 911.
Get Involved in Arthritis Research
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.