If your knee arthritis has gotten so bad that your medication and physical therapy are no longer enough to keep the pain at bay or prevent mobility issues, it is a good time to consider knee replacement surgery. The procedure has come a long way from the extended hospital stays, bed rest, and narcotics-based pain relief of the past.
“Fifteen to 20 years ago we told patients to wait until they could no longer take the pain of osteoarthritis to consider surgery, but that’s not the case anymore,” says P. Maxwell Courtney, MD, assistant professor of orthopaedic surgery at the Rothman Orthopaedic Institute at Thomas Jefferson University Hospital in Philadelphia. “With today’s advances, minimally invasive techniques, and accelerated rehab and recovery protocols, we now tell patients if the pain is limiting your daily activities and you’ve exhausted conservative options — like injections and physical therapy — it’s time to consider surgery.”
That was certainly the case for Sharon Barnes, a teacher from Maine whose pain got so bad she couldn’t sleep. “My doctor said I had osteoarthritis in both knees; it was literally bone on bone,” she remembers. “We did hyaluronic acid injections, and that got me about a year then didn’t work as well. That’s when we started discussing surgery.”
What the Procedure Is Like
Also called arthroplasty, knee replacement is a procedure to resurface the damaged parts of your knee that have been causing you pain.
The knee is the meeting place for three basic bones: the tibia (shin bone) and femur (thigh bone) meet at the joint and are each capped with cartilage to absorb the shock of everyday movement. Resting between them is a freestanding bone called the patella (kneecap). Often using a spinal anesthetic — like an epidural used in childbirth — a knee replacement procedure involves an incision over the knee that allows your surgeon to resurface the tibia, femur, and patella with metal and plastic components to restore the cushioning you need to move your knee comfortably.
There are two general kinds of knee replacement surgery: partial and total.
In a partial knee replacement (also called a unicompartmental knee replacement), only a portion of the knee joint is replaced. This procedure may be recommended for patients who have damage limited to just one area of the knee. Because a partial knee replacement is done through a smaller incision, the recovery time in the hospital is often shorter and people can resume their usual activities sooner. However, more surgery may be needed in the future if other parts of the knee become damaged.
In a total knee replacement, more surfaces of the knee are replaced. Only a small percentage of patients may be good candidates for a partial knee replacement, according to the American Academy of Orthopaedic Surgeons. Most patients have two or more areas of the knee that are damaged, so a total knee replacement is the better procedure for them.
Your surgeon will discuss which type of surgery is right for you based on your medical history and risk factors.
Before surgery, Michael L. Parks, MD, associate professor at the Hospital for Special Surgery in New York City hears a number of common concerns from his patients, such as how much pain they’ll feel and how much they’ll have to depend on others after the procedure. While it’s impossible to anticipate every development, he is happy to reassure them that these days, hospitals are proactive about managing post-operative pain.
While patients will need help in the first weeks after surgery, most people will get their feet under them and regain independence at about six weeks after the procedure.
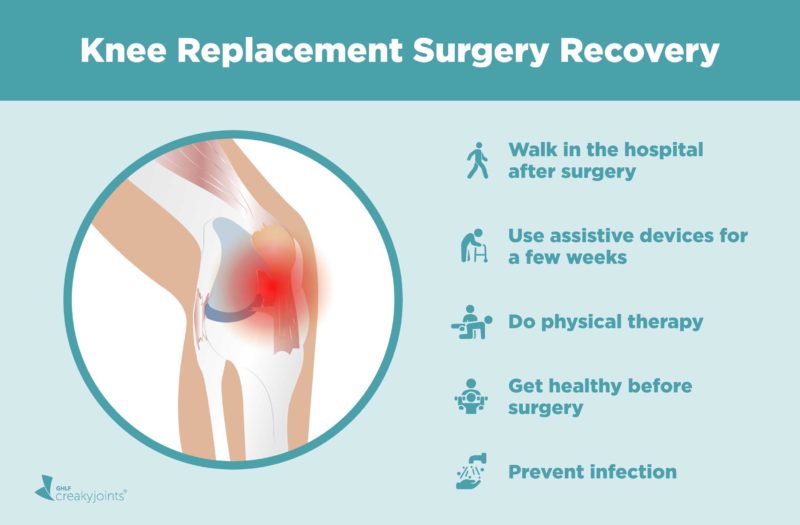
Knee Replacement Recovery Starts Right Away in the Hospital
These days, a typical inpatient stay following knee replacement surgery lasts two days, although some patients go home the same day as surgery, and some patients may need to stay longer.
When thinking about getting back on your feet, it’s helpful to consider the recovery process in phases, beginning immediately after surgery. Health care teams are proactive about keeping patients comfortable for recovery by administering medications such as low-dose narcotics, nerve pain medication, and anti-inflammatory medication. From there, it’s all about getting your knee joint moving again.
“Physical therapy starts the day of surgery and could be as minimal as dangling your feet over the side of the bed,” says Dr. Parks. The remainder of your hospital stay will likely involve physical therapy focused on “activities of daily living,” which you’ll need to move around your home.
“Our physical therapist sees patients the same day as surgery to get them up and walking around the nurses’ station,” adds Dr. Courtney. “It’s no longer about bed rest like it used to be. Now we get patients moving a lot quicker.”
Indeed, Barnes remembers that the hospital staff had her up and moving almost immediately. “I started walking the day of surgery,” she says.
Knee Replacement Recovery Continues Once You’re Home
Even though hospital stays for knee replacement surgery are shorter than they used to be, getting back on your feet still takes time, says Dr. Parks.
The next phase of recovery continues at home, as patients begin acclimating to normal activities, such as moving between rooms, getting up and sitting down in furniture, and using the bathroom. While everyone is different, many patients are likely to have similar experiences during the early weeks of recovery.
For Barnes, stability was a big issue. “I became very aware of where I was placing feet, for example, when stepping off a curb. I just felt a little clumsy early on after surgery so I was afraid of falling.”
In addition, she experienced a lot of swelling. “The hospital gave me a special brace that circulates cold water around the knee, which was great and helped with swelling,” she says.
Whether your doctor has prescribed formal outpatient physical therapy or has entrusted you with an at-home regimen of walking and exercises, patients progressing through recovery achieve some big milestones along the way.
Assistive Walking Devices
In terms of walking without assistance, Dr. Courtney sees most patients need a walker for a few days, then they need a cane for up to six weeks. “By three months most patients are feeling very good,” he adds.
Dr. Parks generally sees his patients walking smoothly at about six weeks. “Many will have a cane, but they’re not dependent on it,” he says. “Even though they may still feel some stiffness and discomfort, I see them moving and straightening their knee nicely at six weeks.”
For Barnes, she felt most comfortable adding an intermediary step between walker and cane. “When it was time for me to move on from a walker, I transitioned to walking sticks, which felt steadier than a cane,” she remembers.
Driving
As for driving, the timeframe can vary. If the left knee is replaced, you may wait two to three weeks before driving; if the right knee is replaced, you may wait three to six. Just be sure you’re no longer taking narcotic medication before getting behind the wheel.
“Brake reaction time is last to come back,” says Dr. Courtney. “So it’s best to have someone in the car with you at first, so you can feel what it’s like to stop at a stop sign.”
Returning to Work
Many patients are eager to hear when they can return to work, but the answer often depends on the occupation. If you have a desk job that allows you to sit comfortably, you may return to work in two to four weeks, says Dr. Courtney. However, if your job requires you to be on your feet a lot, your return may be closer to six weeks. If your occupation entails significant manual labor, you may be staying home for up to two months.
Exercise and Physical Activity
The final phase of recovery, as Dr. Parks considers it, is returning to exercises and extra activities, including hiking and biking. “It typically takes eight to 12 weeks to get to this phase,” he says.
In terms of full knee replacement recovery, patients generally need a year to completely heal and regain total function.
“After a couple of years, you forget that you’ve even had knee surgery,” says Barnes, who would go on to have her left knee replaced a year after the surgery on her right. “Before surgery I couldn’t garden. Now I walk, snow shoe, and climb ladders. I do what I want and don’t have pain.”
Factors That Affect Knee Replacement Recovery
A number of things impact the pace and ease of your recovery, but none as much as your general health and activity level before surgery. “Healthier, more active people tend to recover more quickly,” says Dr. Courtney.
Physical Therapy
In addition, Dr. Parks is a big fan of formal physical therapy. “The big thing is to move,” he says. “I think in some cases formal physical therapy after knee replacement surgery can be as important as the operation itself.”
What’s more, successful pain management paves the way for better recovery, says Dr. Parks, who points out that people who are feeling a lot of discomfort can’t progress well with physical therapy.
Social Support
It’s also a good idea to have family and friends lending a hand throughout your recovery process. “Social support affects recovery success,” says Dr. Parks. “It’s always helpful for family members or a social system to be supporting a patient.”
Motivation to Regain Physical Function
And finally, Dr. Courtney sees another factor speeding recovery for certain patients. “Motivation is big one, especially with knee replacement surgery,” he says. “If patients are involved in sports, like golf, tennis, or swimming, their motivation to get back to their activities plays an important role.”
Preventing Infection
Though post-surgical infections are not common, it is important to take precautions to prevent them. According to the American Academy of Orthopaedic Surgeons, roughly one in 100 people may develop an infection after a joint replacement surgery. Your surgeon will work with you before and after the surgery on steps to prevent infection, such as using a chlorhexidine solution when you shower in the days leading up to the surgery, taking antibiotic medications after the procedure, and being aware of signs of infection in order to treat promptly.
Tips for a Smoother Recovery
Physicians and patients share their insights for safely and efficiently getting back on your feet:
“If you have concerns or if you’re experiencing something you don’t understand, speak up. Your doctor and physical therapist will know if it’s normal or not. In my case I mentioned a muscle spasm issue to my physical therapist, and she got on the phone with my doctor and I ended up needing a medication change to address it.” — Patient Sharon Barnes
“Walking is the best therapy you can do. Walking in the park or around your neighborhood is really how you’ll be able to get back to normal life quicker.” — Dr. Courtney
“I’ve had both [knees] done, 14 and 15 years ago. Best advice: Do your before exercises and build up your strength, then after surgery, do your exercise as soon as you’re able and keep doing them to get your best range of movement. It’s going to hurt, but it’s so worth it. Healing pain is different, it’s pain with an end in sight. My father-in-law told me before I had my first one done, to remember, short-term pain for the long-term gain, and that was my mantra.” — Patient Kathy M., via Facebook
“Keep that knee moving! Don’t use your surgery as an excuse to sit on the sofa all day. You have to get up and walk. Do all of the exercises and stretches you physical therapist gives you and push yourself to make gains every time you go to PT. But don’t overdo it. Listen to your body. It will be painful at first but the more you move, the better you’ll be.” — Courtney M., via Facebook
“I had bilateral knee replacements done two years ago. My advice? Build up your leg muscles before surgery. I started three months before so the muscles were in tip-top shape. It made a huge difference in making therapy so much easier. — Cheryl W., via Facebook
“It’s 90 percent a mental process to buy into the rehab work and think positively. Set a goal. Mine was to return to work after one month and I was able to do that. Love your ice machine for as long as you want. I still use one for residual nerve pain when needed.” — Barin N., via Facebook
“Had both my knees done 10 and 11 years ago. Ice will be your friend! Use it all the time; it helps with any pain you are having. And make sure you do ALL of your physical therapy. It does help to get up back on your feet!! I have had no pain or problems for all these years. And I am 72 years old.” — Elaine M., via Facebook
“I had both of my knees replaced within three months. One was bone on bone and the other had a little remaining cartilage but more painful than the other one. Common sense but these are my tips: 1) Find an amazing surgeon that you trust implicitly or at least was referred via a known reputable source. 2) Know your recovery plan options re: physical therapy. Some people have to go to an inpatient facility due to living alone and not having 24/7 help that first week or so. 3) Do the work with PT so you can get back on your feet safely and ASAP. 4) Get rest. 5) Trust that your new knee(s) will be lifechanging.” — Janine T., via Facebook
Not Sure What’s Causing Your Knee Pain?
Check out PainSpot, our pain locator tool. Answer a few simple questions about what hurts and discover possible conditions that could be causing it. Start your PainSpot quiz.
Keep Reading
Activities After Knee Replacement. American Academy of Orthopaedic Surgeons. https://orthoinfo.aaos.org/en/recovery/activities-after-knee-replacement.
Interview with Michael L. Parks, MD, associate professor at the Hospital for Special Surgery in New York City
Interview with P. Maxwell Courtney, MD, assistant professor of orthopaedic surgery at the Rothman Orthopaedic Institute at Thomas Jefferson University Hospital in Philadelphia
Joint Replacement Infection. American Academy of Orthopaedic Surgeons. https://orthoinfo.aaos.org/en/diseases–conditions/joint-replacement-infection.
Knee replacement. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/knee-replacement/about/pac-20385276.
Knee Replacement Surgery Procedure. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/knee-replacement-surgery-procedure.
Total knee arthroplasty. UpToDate. https://www.uptodate.com/contents/total-knee-arthroplasty.
Total Versus Partial Joint Replacement: What Are the Differences? American Academy of Orthopaedic Surgeons. https://orthoinfo.aaos.org/en/treatment/ortho-pinion-total-vs-partial-joint-replacement.