Your hip or shoulder is achy, stiff, or feels inflamed. When you try to move it, the pain intensifies. You’re wondering what’s going on with your body. Well, it could be any number of problems, but arthritis and bursitis are among the most common contenders. Yet many people don’t understand the difference between arthritis and bursitis and, therefore, can’t begin to figure out which condition they may have.
Arthritis and bursitis both cause painful inflammation that can be perceived as coming from a joint, like your hip or shoulder. The key difference comes down to the specific structure within your body that has become inflamed, and you need to sort it out to get the right treatment.
If you’ve only recently started experiencing discomfort, it’s probably okay to start by resting the impacted area and taking over-the-counter pain relievers. If that doesn’t help — or if the pain is severe enough to interfere with everyday activities, including sleep — you’ll want to see a doctor.
For best results, you’ll want to seek out a rheumatologist (a doctor who specializes in disorders of the joints, muscles, bones, and connective tissue), an orthopedist ( doctor who focuses on bone problems), or a physical medicine and rehabilitation (PM&R) physician (aka a physiatrist, who treats all kinds of pain).
You won’t be able to diagnose yourself with arthritis vs. bursitis, but having some background knowledge of the two issues, including their symptoms and how they’re diagnosed and treated, can help you be more prepared to see a doctor.
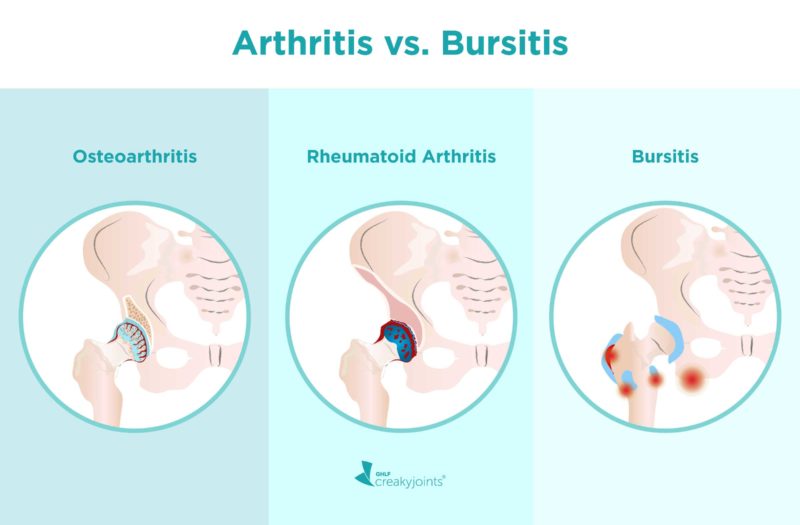
Arthritis vs. Bursitis
Arthritis and bursitis can cause very similar symptoms, though the root causes are different. “Arth refers to joint and itis means inflammation,” explains rheumatologist Joseph E. Huffstutter, MD, a partner with Arthritis Associates in Hixson, Tennessee. “If you’re talking about pure arthritis, the problem is confined to the joints or one particular joint.”
There are more than 100 types of arthritis, but most fall into one of two main categories.
- Osteoarthritis (OA) is a “wear-and-tear” disorder that occurs when the cartilage that cushions joints wears down over the years.
- Inflammatory arthritis (IA), which includes rheumatoid arthritis (RA) and psoriatic arthritis (PsA), among others, occurs when the body’s immune system mistakenly attacks the joints.
Just as arthritis, by definition, means joint inflammation, bursitis means inflammation of the bursa. Bursa are tiny sacs that are found throughout the body, primarily around joints or tendons. Their job is to help lubricate joints and reduce friction as you move.
“Normally the sacs are empty, but when they become inflamed or irritated they get filled with fluid. When there’s fluid or inflammation, that’s bursitis,” says Dena Barsoum, MD, a physical medicine and rehabilitation physician with the Hospital for Special Surgery in New York City.
Both arthritis and bursitis can cause similar symptoms, which is why it can be difficult to figure out what’s going on without the help of a doctor. The following symptoms around a joint may indicate either arthritis or bursitis:
- Pain
- Swelling
- Redness
- Warmth
In some cases, the area of your body that’s in pain might provide some clues about the cause. Bursitis, for instance, can occur anywhere you have bursa, but large joints like the shoulder and hip, which have a large range of motion, are common spots for bursitis flare-ups.
Inflammatory arthritis like RA can affect these spots, too, but the disease tends to cause pain in several areas at once, so you might have pain in both hips, or in your hip as well as your knee. Another difference: RA tends to be accompanied by some non-joint symptoms, such as unexplained fevers and extreme fatigue. While bursitis can present more like an injury that pops up suddenly and lasts for days or weeks, osteoarthritis tends to come on slowly and never go away.
Risk Factors for Bursitis
Anyone can get bursitis, but certain factors make it more likely. You’re more likely to develop bursitis if you:
- Are over age 40, as risk increases with age
- Participate in sports or activities that repeatedly strain an area of the body where you have bursa, such as your shoulder
- Are a “weekend warrior” when it comes to exercise. Being mostly sedentary and then suddenly overdoing it often leads to bursitis, says Dr. Huffstutter.
- Are overweight, since excess weight puts pressure on bursa, as well as the joints themselves)
- Have arthritis. Because both conditions have to do with the joint (or, in the case of bursa, a structure that lubricates the joint), they often overlap. Several types of arthritis, including RA, OA, and gout, may increase the risk of bursitis.
Most of these risk factors for bursitis also pertain to arthritis. For example, RA is usually diagnosed during middle age, and OA may develop after years of physical activity that causes cartilage to wear down. People who are overweight are also more prone to various types of arthritis, including RA, OA, and gout.
Does Bursitis Cause Arthritis — and Vice Versa?
Bursitis does not cause arthritis. The reverse isn’t true either, though having arthritis does make getting bursitis more likely.
“You commonly see them together. For instance, if a person develops arthritis in their shoulder, they might change the way they use their shoulder, which could lead to bursitis,” says Dr. Huffstutter. “Or people develop arthritis in their knee or hip, which changes their gait” and irritates the bursa in that area.
How Is Bursitis Diagnosed?
If you suspect you have bursitis — or if you have pain near a joint and aren’t sure if it’s arthritis or bursitis — a knowledgeable doctor should be able to find an answer. The most crucial step toward getting the right diagnoses is a thorough physical exam and patient history. “The number-one thing is getting a good history from the patient, including what specific movement bothers them and when it bothers them,” says Dr. Huffstutter.
You doctor will likely start the physical exam by asking you to point out where your body hurts. This simple question can provide a lot of insight when it comes to differentiating between bursitis and arthritis. “A lot of times a patient will say, ‘I have pain in my hip,’ and when I say, ‘Where?’ they’ll point to the outside of the joint,” says Dr. Barsoum. “That’s not arthritis. Arthritis pain comes from inside the joint.”
The doctor will then touch the painful area and ask you to move the joint. If you do have bursitis, your doctor may be able feel fluid in a tender spot. “If it hurts when I’m pressing on the area [where I know there’s bursa], then I’ll suspect bursitis,” says Dr. Barsoum. She often then uses an ultrasound to check for the presence of fluid. In some cases, an MRI might also be used to check for inflamed bursa. (X-rays aren’t used to diagnose bursitis, because they only show bone.)
How Is Bursitis Treated?
Fortunately, treatment for bursitis is relatively easy. Some possible treatment options include:
Anti-inflammatory drugs
Over-the-counter oral or topical non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can often help relieve bursitis pain and inflammation, especially when used in conjunction with comfort measures like applying ice to the painful area and resting it.
Cortisone injections
If your case is bad enough that you’ve made it to the doctor’s office, you’ll likely get an injection of cortisone along with lidocaine (a numbing agent) directly into the affected bursa. This is usually very effective because it quickly reduces pain and swelling.
Physical therapy
“There’s a growing body of evidence that some patients can go without the [cortisone] injection if they participate in physical therapy,” says Dr. Huffstutter. “Others need the exercise in addition to the injection.” Physical therapy aimed at strengthening and stretching the surrounding muscles is key because moving it prevents you from further irritating the bursa. Simply moving the joint more, however, won’t necessarily help. “You can do as much harm as good if you’re not moving correctly,” says Dr. Huffstutter.
Fluid aspiration or surgery
These are rarely necessary for bursitis, says Dr. Barsoum, because most patients benefit sufficiently from cortisone injections and/or physical therapy. Most people only need fluid aspiration or surgery if other treatments have failed.
With proper treatment — usually just rest, anti-inflammatories, and maybe an injection and some physical therapy — most people with bursitis feel better within a few weeks. Still, it’s important not to ignore the problem: If left untreated, the bursa may rupture, become infected, or cause bone or muscle problems.
Once you’ve had bursitis, it’s also wise to take steps to avoid a recurrence. Warming up before exercise, giving your body time to acclimate to new activities, and taking rest breaks can help. You can also use a pad or cushion on a bursitis-prone joint whenever you need to put extra pressure on it (like if you have to kneel on your knee).
Not Sure What’s Causing Your Pain?
Check out PainSpot, our pain locator tool. Answer a few simple questions about what hurts and discover possible conditions that could be causing it. Start your PainSpot quiz.
Baker S. Things to Know About Bursitis. Susan Baker, MD. https://www.susanbakermd.com/blog/things-to-know-about-bursitis.
Bursitis. Mayo Clinic. July 31, 2020. https://www.mayoclinic.org/diseases-conditions/bursitis/symptoms-causes/syc-20353242.
Bursitis of the Hip. Family Doctor. https://familydoctor.org/condition/bursitis-of-the-hip/. April 16, 2020
Interview with Dena Barsoum, MD, physical medicine and rehabilitation specialist with the Hospital for Special Surgery in New York City
Interview with Joseph E. Huffstutter, MD, rheumatologist and partner with Arthritis Associates in Hixson, Tennessee
Kotton CN, et al. Septic bursitis. Up to Date. June 29, 2020. https://www.uptodate.com/contents/septic-bursitis.
Treatment for Bursitis. Stanford Health Care. https://stanfordhealthcare.org/medical-conditions/bones-joints-and-muscles/bursitis/treatments.html.
Truong J. Septic Bursitis. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK470331/.