You’ve probably heard of tendonitis, which is the inflammation of a tendon — a cord-like structure that connects muscle to bone. Tenosynovitis also has to do with tendons, but there’s a slight difference: It means inflammation of the tendon sheath.
A sheath is what encloses a tendon. Made of layers of connective tissue and filled with lubricating fluid, a sheath protects the tendon as well as keeps it close to the bone, says Joshua Abzug, MD, Associate Professor of Orthopedics and Pediatrics at the University of Maryland School of Medicine. “Think of it like a wrapper on a straw,” he says.
You’ll find tendons all over your body, but not every tendon has a sheath. Tendons that are enclosed in sheaths are mostly in your hands, wrists, and feet. If one of those sheaths becomes inflamed, you end up with tenosynovitis.
Anyone can develop this problem, but if you have a type of inflammatory form of arthritis, like rheumatoid arthritis or psoriatic arthritis, your risk is higher than average because the same inflammation that impacts your joints can also impact your tendons and the sheaths around them.
Symptoms of Tenosynovitis (Tendon Sheath Inflammation)
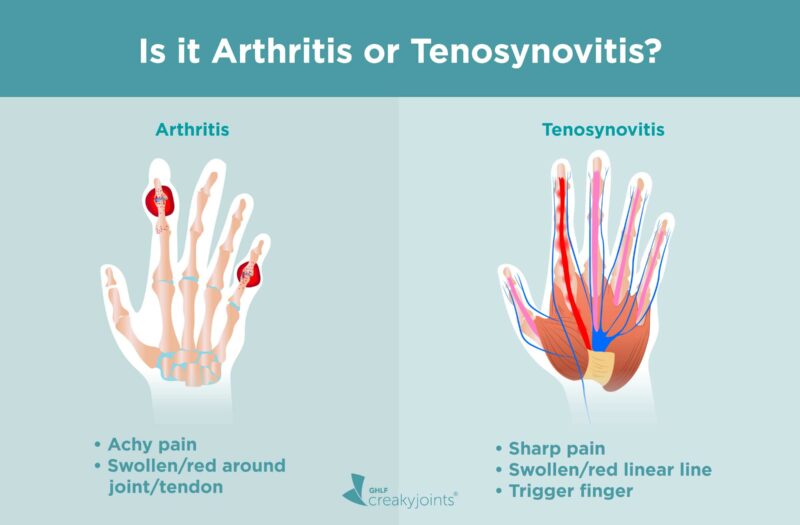
So how do you know if you’re dealing with tenosynovitis or arthritis? It can be hard to tell, especially without the help of a well-trained doctor, says Bonita Libman, MD, Division Chief of Rheumatology & Clinical Immunology at the University of Vermont Medical Center.
While symptoms like pain, swelling, and redness often overlap, there are some clues that point to tenosynovitis:
- Sharp pain: Arthritis pain is more often described as achy.
- Swelling and/or redness that runs in a linear fashion (for example, down the side of your finger): In arthritis, the swelling and/or redness would be concentrated around the knuckle.
- Trigger finger: You feel like your finger locks up or catches when you try to bend and then straighten it.
Does Arthritis Cause Tenosynovitis or Vice Versa?
Tenosynovitis does not cause arthritis, but certain types of inflammatory arthritis can cause tenosynovitis, says Dr. Libman.
Psoriatic arthritis (PsA) and rheumatoid arthritis (RA) are among the most common types of arthritis that may cause tenosynovitis. The reason largely comes down to inflammation. If you have PsA or RA, you have excessive levels of inflammation throughout your body, and especially in structures that are near your joints (including the tendons).
Arthritis also causes degeneration of cartilage that normally cushions joints, so it may change your patterns of movement in such a way that puts extra stress on the tendons and the surrounding sheaths.
Additionally, although tenosynovitis does not directly cause arthritis, it sometimes serves as an early warning sign of the disease. “Developing tenosynovitis does not necessarily mean that you have an autoimmune problem, but if it doesn’t respond to conservative care [like ice and rest] — and you have no history of overuse or trauma — you should be evaluated to see if you might be developing one,” says Dr. Libman.
In fact, research has found that psoriasis patients who get tenosynovitis are more likely than others with psoriasis to develop PsA. Different studies have found that tenosynovitis coupled with a positive rheumatoid factor antibody test is a strong predictor of early RA.
Other Causes of Tendon Sheath Inflammation
However, inflammatory arthritis is not the only cause of tenosynovitis. Most people who have tendon sheath inflammation are not on their way to developing arthritis, says Abzug. In the general population, the most common causes of tenosynovitis are:
- Aging. The tendon sheath gets a little smaller as you get older. “If the tendon gets inflamed or thickens, there’s less room for it” within the sheath, says Dr. Abzug.
- Certain medications. Antibiotics in the fluoroquinolone class (such as Cipro) may damage tendons and cause problems including tenosynovitis. Tenosynovitis may also be a rare side effect of statins (cholesterol-lowering medication).
- Diabetes. Chronically high blood sugar can damage tendons and make tenosynovitis more likely.
- Repetitive motion. Knitting or playing video games can lead to tenosynovitis in the sheath that encloses the tendon that runs from your wrist to your thumb. Tenosynovitis in this area is known as De Quervain’s tenosynovitis, and it’s also common in new mothers because they’re frequently lifting a baby.
Diagnosis
If you’re already living with inflammatory arthritis and think you might have tenosynovitis, talk to your rheumatologist. People who don’t have arthritis should start by consulting their primary care physician or an orthopedist, with an important exception: If the problem seems to be occurring in multiple areas like in your fingers and feet — and there’s no clear reason why (you don’t have a known trauma or overuse of those areas) — you should be screened by a rheumatologist, says Dr. Libman.
To diagnose tenosynovitis, your doctor should perform a through physical exam. This might entail pressing on certain spots to try to pinpoint the source of the pain. Your doctor might also ask you to bend the impacted area in a specific way to test your range of motion and pain level.
You probably won’t need imaging tests, though in certain cases an MRI is needed to confirm the diagnosis.
Treatment
Most people with tenosynovitis can start with rest, ice, and over-the-counter anti-inflammatory medication, says Dr. Libman. If you’ve done that for two to four weeks and it’s not improving — or if the pain is very severe — it’s time to see a doctor.
If you have inflammatory arthritis, developing tenosynovitis suggests that your current medication regimen might need a tweak. After evaluating you, your rheumatologist might add or change a medication to better control your condition.
Whether or not you have arthritis, specific treatments for tenosynovitis may include:
- Stronger anti-inflammatory drugs. Your doctor might recommend prescription anti-inflammatories to reduce pain and swelling.
- Splint. Immobilizing the joint that’s associated with the impacted tendon can help it rest so it can heal.
- Physical therapy. Your provider might suggest specific stretching and/or massage techniques.
- Cortisone injections. Administering medication into the sheath can help control inflammation.
- Surgery. It’s a last resort, says Dr. Abzug, but if other options fail and you’re in a lot of discomfort then surgically removing some tissue can help by giving the tendon more room to move.
Can Tenosynovitis Be Prevented?
Once you’ve had tenosynovitis, it makes sense to be concerned about getting it again. If you have inflammatory arthritis, your best move is to focus on keeping your disease activity low, as that will reduce inflammation throughout your body.
If your tenosynovitis was caused by repetitive motion, trying to minimize movement that stresses the same body part is wise. If the problem occurred in a finger, for instance, limit activities like gardening and knitting that call for repetitive hand motions. While certain activities — like picking up your baby — are unavoidable, ask your doctor or physical therapist for guidance on doing them in a way that’s less likely to put pressure on the impacted tendon.
American College of Cardiology. Statin Safety and Adverse Effects. https://www.acc.org/latest-in-cardiology/articles/2018/12/12/07/23/statin-safety-and-adverse-events.
Interview with Bonita Libman, MD, Division Chief, Rheumatology & Clinical Immunology, at the University of Vermont Medical Center.
Interview with Joshua Abzug, MD, Associate Professor of Orthopedics and Pediatrics at the University of Maryland School of Medicine.
Inserro A. Development of PsA Linked to Tenosynovitis in Patients With Arthralgia. The American Journal of Managed Care. November 2019. https://www.ajmc.com/view/evaluating-treatment-goals-preferences-in-parents-and-young-patients-with-psoriasis.
Institute for Quality and Efficiency in Health Care (IQWiG). What are tendons and tendon sheaths? July 2018. https://www.ncbi.nlm.nih.gov/books/NBK525770/.
Nieuwenhuis WP, et al. Evaluation of magnetic resonance imaging-detected tenosynovitis in the hand and wrist in early arthritis: mri-detected tenosynovitis in early arthritis. Arthritis & Rheumatology. 2015. doi: https://doi.org/10.1002/art.39000.
NYU Langone Health. Diagnosing Wrist & Hand Repetitive Use Injuries. https://nyulangone.org/conditions/wrist-hand-repetitive-use-injuries/diagnosis.
Rees J, et al. Rehabilitation of tendon problems in patients with diabetes mellitus. Metabolic Influences on Risk for Tendon Disorders. 2016. doi: https://doi.org/10.1007/978-3-319-33943-6_19.
Sahbudin I, et al. The role of ultrasound-defined tenosynovitis and synovitis in the prediction of rheumatoid arthritis development. Rheumatology. April 2018. doi: https://doi.org/10.1093/rheumatology/key025.