Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic inflammatory disease that causes pain, stiffness, swelling, and loss of function in joints throughout the body. It typically first affects the small joints of the hands and feet.
Rheumatoid arthritis is an autoimmune disease. This means that your immune system, which is supposed to protect against germs and foreign invaders, turns against the body and starts attacking itself. This causes inflammation that can affect not only the joints, but also such organs as the heart, lungs, eyes, and more. RA can strike at any age although it usually begins between the ages of 40 and 60. RA is more common in women than men. Early diagnosis of rheumatoid arthritis is important because it can damage your joints and organs if left untreated.
Learn more here about how to manage rheumatoid arthritis.
Rheumatoid Arthritis Basics
Causes of Rheumatoid Arthritis
Most experts believe that a variety of factors conspire together to create the perfect storm that eventually triggers RA to develop. Here’s a look at some of the most important RA risk factors ones that might raise your odds of developing this condition.
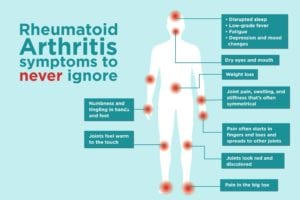
Rheumatoid Arthritis Symptoms
While rheumatoid arthritis can affect each person differently, there are common symptoms that affect nearly all patients, as well as lesser-known symptoms that can also provide clues to diagnosis. Here are some RA symptoms you need to be aware of. Some are specific to the joints, while others are more systemic.
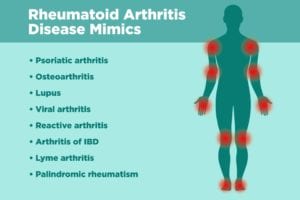
Diseases That Could Mimic RA
Viral infections, other kinds of arthritis, and other autoimmune diseases may all be mistaken for RA, depending on which specific constellation of symptoms you have. It’s important to learn about these different diseases so you can be sure to be as specific as possible when describing your medical history to your doctor.
Seeing a Rheumatologist for RA
The sooner you see a specialist and get the right diagnosis, the sooner you can start treatment that will keep you active, healthy, and pain-free. Since RA is the most common type of inflammatory arthritis rheumatologists tend to see, most specialists will have plenty of experience treating RA. Here are some tips to help you make the most of that first visit to a rheumatologist.
Rheumatoid Arthritis Diet
Figuring out what to eat — and what not to eat — with rheumatoid arthritis is admittedly tricky. Learn about eating a healthy diet for rheumatoid arthritis from nutritionists who live with RA themselves.
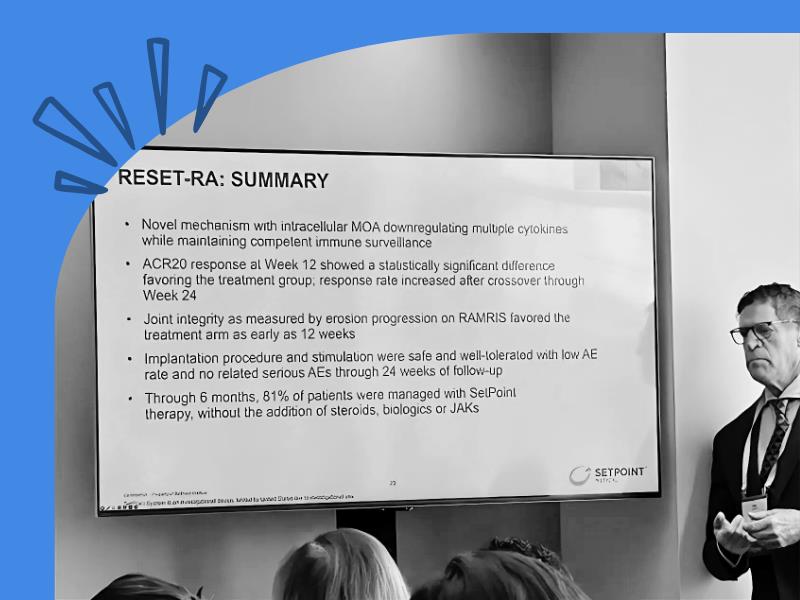
RA Treatment & Medication
There are a variety of rheumatoid arthritis medications your physician may prescribe. These medications will work differently for each individual. Learn more about available RA treatments.
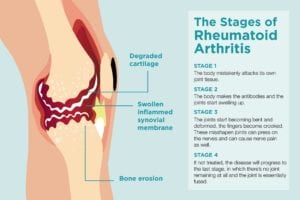
Stages of RA Progression
Early treatment for RA is key, because whatever joint damage has already occurred can’t be reversed. Find out how to recognize the symptoms at each stage of RA, and what can be done to treat it.
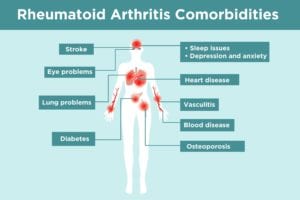
Rheumatoid Arthritis Comorbidities
As a patient, it’s important to understand all the possible rheumatoid arthritis comorbidities and complications so you can try to prevent them and watch for early signs and symptoms. Once you read through this list of RA complications, bring up any questions or concerns you have with your doctor.
Download the RA Patient Guidelines
With the help and guidance of our Patient Council (a group of patient leaders from across the country), we have published the first comprehensive document that helps all individuals during their RA disease journey.
Remission and Low Disease Activity in RA
Remission (inactive disease) or low disease activity (LDA) is a state that keeps your symptoms under control and helps maintain a good quality of life. Learn how achieve them if you have RA.
Most-Read Rheumatoid Arthritis Articles
These 15 Myths About Rheumatoid Arthritis Can Be Downright Dangerous to Believe
These stubborn myths aren’t just annoying to patients who know better; they are risky to believe for people who are just starting to learn more about their disease.
How I Explain What Rheumatoid Arthritis Actually Is to People Who Don’t Have It
Eileen Davidson, 33, knows it’s not easy for others to understand what it’s like to live with RA. Here’s how she attempts to describe it.
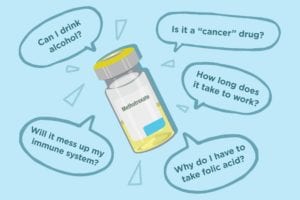
11 Common Questions About Taking Methotrexate for Rheumatoid Arthritis
It’s normal to have questions (okay, a lot of questions) about taking methotrexate. Is it really a cancer drug? Can you drink alcohol? Get answers here.
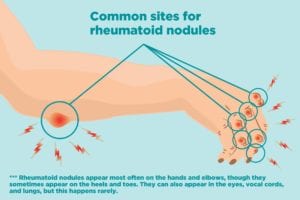
What Are Rheumatoid Nodules? 5 Key Questions and Answers for RA Patients
Rheumatoid nodules are becoming less prevalent, but here’s what you need to know about what causes them and how to treat them.
12 Surprising Upsides of RA You Might Not Have Considered
As awful and scary as RA is, there are some surprising benefits to having it, from being a better health advocate to eating better. Here are benefits you may not have considered.