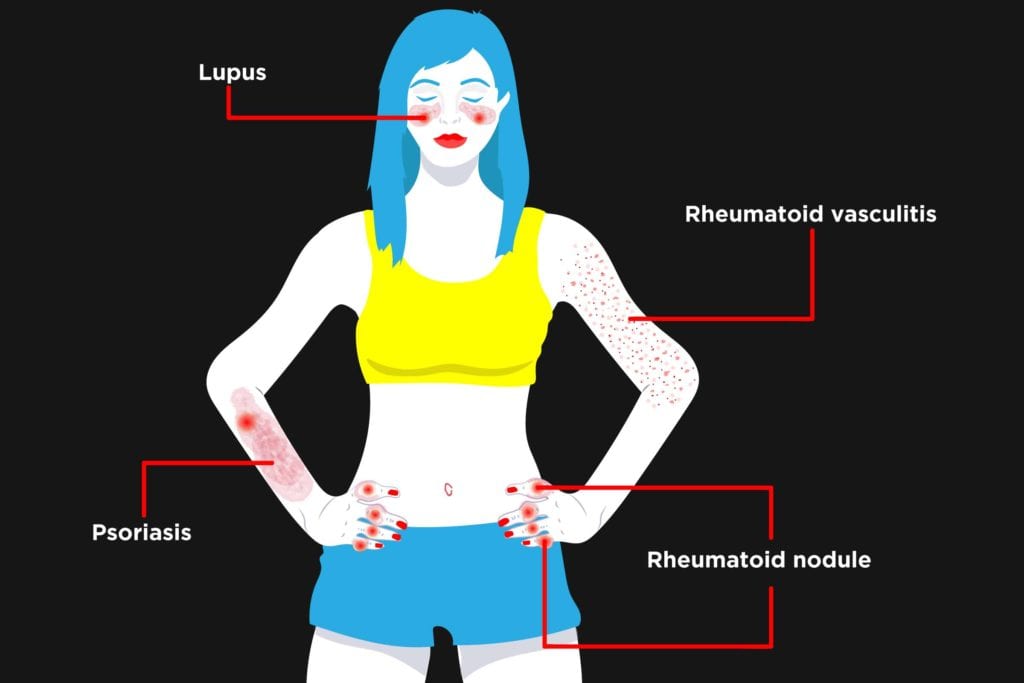
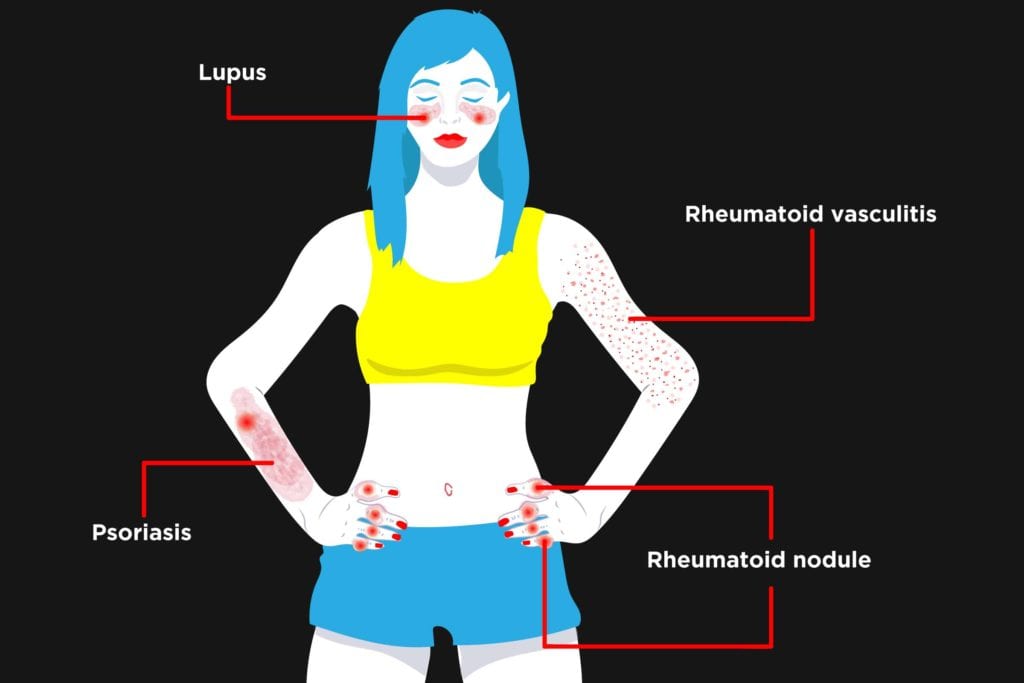
Before the modern era of treating rheumatoid arthritis (RA) early with disease-modifying drugs, you could often guess that a person had RA just by looking at their skin. Long-term, severe rheumatoid arthritis damages small blood vessels throughout the body. This condition is called rheumatoid vasculitis, which shows up as bruising, pain, and sores on the skin. Another telltale sign of RA used to be rheumatoid nodules under the skin, often near affected joints.
“We used to see nodules a lot, but these lumpy bumps — about the consistency of a pencil eraser — are getting less common with better therapy,” says rheumatologist Kevin Deane, MD, PhD, associate professor of medicine at the University of Colorado School of Medicine.
While, thankfully, these skin conditions are no longer as common as they used to be, many people with RA can develop skin problems that raise questions about whether and how they might be related to their arthritis.
3 Ways RA Can Lead to Skin Eruptions
1. Out-of-whack immune system. In RA, your immune system has already attacked your own joints. This revved-up immune system can also be related to eczema or allergies that affect the skin, says Dr. Deane.
2. Tamped down immune defenses. Dampening your immune system with medication can help control your RA symptoms, but they may leave your skin more vulnerable to infection, Dr. Deane cautions.
“If you have a rash that’s rapidly spreading, is bright red, or is accompanied by fever or malaise, we think about infections such as cellulitis — a potentially dangerous bacterial infection of the skin,” says Dr. Deane.
3. Other medication reactions. Rashes can occur at the site where you inject a biologic medication. These are usually mild and clear up in a few days. More worrisome are overall rashes or hives that appear during or within 24 hours after you receive infusion of a drug directly into your bloodstream.
“Unfortunately, there’s a rare but real chance for an allergic-type reaction from infusions of RA medications. These usually appear within 12-24 hours of the infusion and need immediate medical attention,” Dr. Deane says.
Several drugs that are used to treat RA, including TNF inhibitors, may sometimes induce or worsen psoriasis, a skin disease that creates an itchy scaly rash (more on that below).
Long-term use of corticosteroids, such as prednisone, can also leave the skin more prone to bruising or tears.
And while the frequency of skin nodules due to RA has diminished overall, in rare cases medications such as methotrexate cause multiple nodules to appear on the feet, hands, or ears.
When Your RA Skin Rash Could Actually Mean a Different Diagnosis
There’s lots of overlap in symptoms between various types of arthritis. Even if you’ve already been diagnosed with RA, your rheumatologist may reconsider your diagnosis if you develop certain telltale skin signs.
- A butterfly-shaped rash on your cheeks and across the bridge of your nose will raise the possibility of lupus.
- A scaly rash may point towards psoriatic arthritis.
“If someone with a diagnosis of RA come in with a scaly rash, especially on the elbows, knuckles, behind the ears, scalp, or along with changes in their fingernails, we’ll think about psoriasis and psoriatic arthritis,” says Dr. Deane.
Getting the Right Treatment for an RA Skin Rash
Who do you call when your skin flares? For people with psoriatic arthritis, considering skin and joint problems in tandem makes so much sense that more than two dozen combined dermatology/rheumatology clinics have been established.
For RA, the director of the combined Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital in Boston suggests contacting your rheumatologist.
“Starting with the rheumatologist who is treating your joint disease and prescribing your arthritis medication would be a good first step. They can decide if a dermatology referral is appropriate,” says Joseph F. Merola, MD, who is also an associate professor of dermatology at Harvard Medical School.
If you can, snap a picture of the problem area on your phone and bring it to your appointment.
“I would still want to examine you in person, but it can be very helpful for me to see a picture of how the rash looked early on,” says Dr. Deane.
Accurately diagnosing a skin problem sometimes requires a skin biopsy, blood tests, or allergy tests in addition to a physical examination. Once your doctor has pinpointed the problem, the answer may be a specific skin remedy or adjusting your arthritis regimen.
“If your skin rash seems to be related to your medication, the rheumatologist and dermatologist, together with you, will decide on whether it makes the most sense to continue the current therapy, add a medication to the regimen to control skin disease, or potentially change to a different arthritis medication to control the symptoms of both the skin and joint disease,” says Dr. Merola.
How to Help Prevent RA Skin Problems
1. Protect skin from the sun
Using sunscreen and minimizing exposure is more important if you have RA because your risk of some types of skin cancers may be increased, especially if you take methotrexate or a TNF inhibitor. Your arthritis medications may also make your skin more sun sensitive, says Dr. Deane. See a dermatologist for a thorough skin check every year.
Don’t smoke
While rheumatoid vasculitis has become less common in recent years, large studies from the Mayo Clinic and Sweden reveal smokers have a higher risk. Smokers are also more likely to develop psoriasis as a side of effect of RA treatment with TNF inhibitors.
3. Ask about shingles vaccine
People with rheumatoid arthritis are about twice as likely as other adults to develop shingles, a painful and sometimes dangerous rash that can occur when the virus lingering from a previous chickenpox infection (herpes zoster) is reactivated in the body. Talk to your rheumatologist about whether, when, and what type of shingles vaccination might be advisable for you: There’s no one-size-fits-all guideline yet on which individuals with RA should be vaccinated against shingles, and there are now two types of vaccines available that have different rules surrounding their use, Dr. Deane says.





