This story includes mention of suicidal ideation, which may be disturbing to some readers. If you or someone you know need help, consider calling the National Suicide Prevention Hotline at 800–273–8255 or the Trevor Project Hotline (for LGBTQ+ youth) at 866–488–7386.
Key Takeaways
- Depression and suicidal thoughts affect people with psoriasis and psoriatic arthritis, but there may be additional or more severe issues for people with PsA.
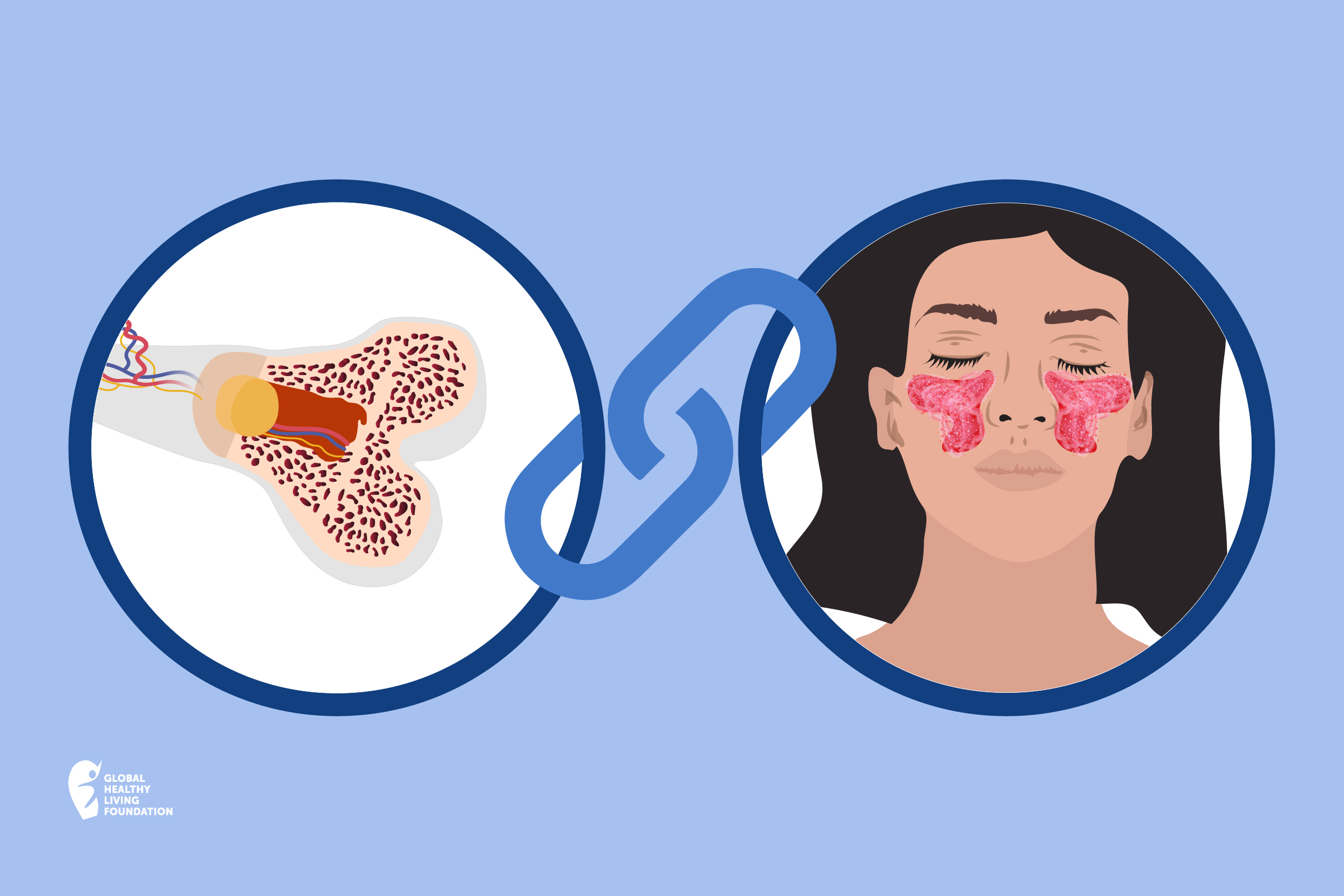
- Inflammation and pain associated with PsA might cause both functional impairments and brain changes that make depression and suicidal tendencies more likely.
- Screening for depression is very important for people with psoriasis and PsA.
Many people with psoriasis have depression, and the reasons are complex. While some struggle with poor self-image, embarrassment, and fear of being rejected by others because of the appearance of their skin, there’s also evidence that inflammation plays a role in both conditions.
A new study suggests that people with psoriatic arthritis (PsA) — a disease that combines joint inflammation with skin lesions — are even more prone to depression than those who have psoriasis alone.
The study, conducted by researchers in the UK, entailed surveying 219 patients with chronic plaque psoriasis. Of that group, 84 had also been diagnosed with PsA. The researchers, writing in the Journal of the Academy of Consultation-Liaison Psychiatry, measured depression using standardized assessments related to mood.
According to the findings, depression was common in both groups. About half of all participants reported having thought about suicide at some point in their lives. However, those with PsA were significantly more likely to report having thought about suicide recently (within a week of the study). The PsA patients also reported more anxiety and lower “hedonic tone,” meaning a reduced ability to feel pleasure.
The authors theorized that the inflammation and pain associated with PsA might cause both functional impairments and brain changes that make depression and suicidal tendencies more likely.
These findings “highlight the need for routine depression screening in patients with psoriasis, particularly when PsA is present and during painful flares,” the authors wrote, adding that depression often goes undiagnosed. “A PsA diagnosis should trigger depression screening, regardless of comorbidities, psoriasis severity or [how patients rate their overall quality of life].”
Found This Study Interesting? Get Involved
If you are diagnosed with arthritis or another musculoskeletal condition, we encourage you to participate in future studies by joining CreakyJoints’ patient research registry, ArthritisPower. ArthritisPower is the first-ever patient-led, patient-centered research registry for joint, bone, and inflammatory skin conditions. Learn more and sign up here.
Lada G, et al. Depression and Suicidality in Patients with Psoriasis and the Role of Psoriatic Arthritis: A Cross-sectional Study in a Tertiary Setting. Journal of the Academy of Consultation-Liaison Psychiatry. January 2022. doi: https://doi.org/10.1016/j.jaclp.2021.12.007.
Sahi FM, et al. Association Between Psoriasis and Depression: A Traditional Review. Cureus. August 2020. doi: https://doi.org/10.7759/cureus.9708.