Learn more about our FREE COVID-19 Patient Support Program for chronic illness patients and their loved ones.
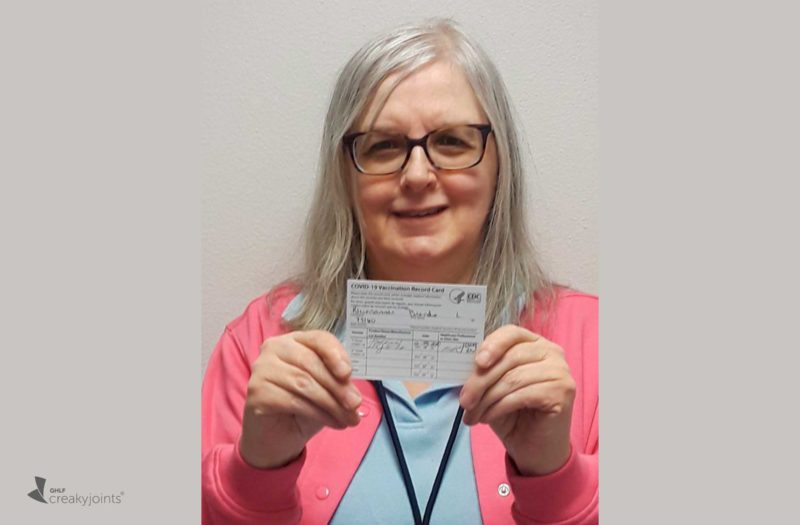
Brenda Kleinsasser, 60, is still surprised — but ever so grateful — that she was able to get the Moderna COVID-19 vaccine this week. “I figured it would be limited to doctors and nurses — I didn’t think it would be available to people like me just yet,” she says.
Brenda works at a large medical practice in Bismarck, North Dakota in the medical records department. She goes to work in person every day — and has throughout the entire pandemic — in the office’s business services department, with about 20 other people. They sit in cubicles and are required to wear masks when they leave their desks or are in shared spaces, like the break room.
Thankfully, Brenda doesn’t interface directly with patients who have COVID-19, but she has plenty to worry about because of the high rates of COVID-19 in her state and her personal risk factors.
North Dakota infamously became the country’s top coronavirus hotspot this fall, with the most COVID-19 cases and deaths per capita. The state was among the last to implement a statewide mask mandate (it was first issued in mid-November) and other restrictions to help prevent community spread of the coronavirus, such as limiting the capacity of restaurants, bars, and large-scale venues.
Brenda has been concerned about contracting COVID-19 because of her age and her underlying health issues and medications. She has had rheumatoid arthritis for nearly 30 years and takes a biologic, etanercept (Enbrel), which affects immune system function. She is also a brain tumor survivor (she was diagnosed in 2008).
“I lost a friend to COVID recently who is in my same age group,” Brenda says. “He was only 66 and just retired from being a dentist in August. After he got sick, he was hospitalized, on a ventilator, and died of sepsis. It was devastating.”
Even though she works in a health care setting every day, Brenda says she is more concerned about exposure to COVID-19 near her home. She lives in an apartment complex “where lots of children are always running around, and no one wears a mask.” She doesn’t leave her apartment except to go to work, getting her groceries delivered and takeout from a local restaurant once a week to help support local businesses. But she’s observed that oftentimes the delivery people do not wear masks, which makes her uncomfortable.
Deciding to Get the COVID-19 Vaccine
As soon as she started hearing the details about the COVID-19 vaccines — their efficacy, the fact that they are not live vaccines and therefore can be given to people on immunosuppressant medication — Brenda knew she wanted to get one when she could.
“The bottom line: I trust science,” she says. “Being on a biologic medication that’s helped to control my symptoms for almost 20 years has taught me this. I did my research. It was clear that these vaccines underwent a vigorous research process just like biologics do. People may be worried because the vaccines are so new, but they’ve been in development for years. I’m just grateful they became available so quickly. Who would have thought they’d be here before the end of the year?”
When Brenda first heard that her workplace would be getting access to the vaccine, she called her rheumatologist to get his take.
Even though people on biologics were not included in the clinical trials for the vaccine, her rheumatologist did not seem that concerned. He was more worried about her age and the fact that her health issues could put her at increased risk of COVID-19 complications.
“He said, ‘Getting a vaccine is much better than getting COVID-19. I highly recommend you get it,’” Brenda recalls.
What Immunocompromised Patients Need to Know About COVID-19 Vaccines
While it is true that people on immunosuppressant medications were not included in the clinical trials, this is not unusual. These medications are first studied in healthy adults and then are typically studied in special populations (such as the immunocompromised, pregnant or breastfeeding women, or children) once more is generally known about safety and effectiveness.
Because the Pfizer and Moderna vaccines are not live vaccines, there’s no reason to think they would be less safe in people on immunosuppressant medication, though they be may less effective, major medical organizations have stated.
You can read more here about getting the Pfizer vaccine or the Moderna vaccine when you’re immunocompromised.
What Getting the Vaccine Was Like
Brenda found out on Monday, December 28 via a work email that she could get the vaccine later that day. In the afternoon toward the end of her work day, she and some colleagues from her department headed over to a clinic within the medical building.
After waiting briefly, a nurse called people back individually and did a screening to ask about COVID-19 symptoms like fever and cough. They asked if she’d ever had COVID-19 previously, and whether she had any underlying health issues or allergies. Brenda wrote about her rheumatoid arthritis and biologic on her form, but it was not a big point of discussion.
As for getting the shot itself, “I didn’t feel a thing,” Brenda says. “I thought the nurse was still preparing it and it was already done. I barely even noticed it.”
The first two nights after getting the vaccine, Brenda woke up with chills that forced her to bundle up. She had a slight headache the next day and has had soreness in her left arm near the injection site.
What I Want Other People to Know About Getting the COVID-19 Vaccine
“I honestly didn’t think I’d be able to get the vaccine until the spring,” says Brenda. “If you have an opportunity to get it and aren’t sure if you want to, I think you should talk to your health care provider. They can help address and ease your fears. For me, it goes back to trusting science and knowing that this is the only way we’re going to get our life back.”
As for her everyday life, Brenda is expecting to stick with the status quo for some time. “I’m certainly not going to get cocky,” she says. “I’m going to keep doing everything I’ve been doing — wearing my mask, distancing, washing my hands — for the last nine months. But I do feel more relieved and safer.”
A friend who works in a nursing home is hoping to get vaccinated next week. When she and Brenda spoke recently, she said optimistically, “Maybe in a few months we can actually see each other in person again.”
Brenda has seen very few people during the pandemic except for her coworkers. When Brenda’s older sister passed away (from Alzheimer’s disease) in the spring, Brenda didn’t join her other sister, who came in from Kansas, for the funeral.
“I have an underlying health condition and I just can’t go,” she told her at the time. “It’s just the way it is.”
Get Free Coronavirus Support for Chronic Illness Patients
Join the Global Healthy Living Foundation’s free COVID-19 Support Program for chronic illness patients and their families. We will be providing updated information, community support, and other resources tailored specifically to your health and safety. Join now.