Having inflammatory arthritis is a pain in a lot of places: Your hands, your feet, your back, your butt. But did you also know that diseases like rheumatoid arthritis can also have an impact on your oral health?
It’s true that issues such as tooth decay, gum disease, and other mouth troubles are incredibly common in U.S. adults: 90 percent have had at least one cavity, about 4 percent have a mouth sore at any given time, and close to half have periodontitis — an infection in the gums that causes bone loss in the mouth.
But people with certain types of arthritis and related conditions are at increased risk for these and other oral health issues, says rheumatologist Felipe Andrade, MD, PhD, an associate professor of medicine at Johns Hopkins University School of Medicine in Baltimore.
Pain and stiffness in people with arthritis can make brushing and flossing harder to do well. And if you have jaw pain from arthritis, then lying in a dental chair with your mouth wide open for cleaning and exams isn’t exactly pleasant, says Lauren E. Levi, DMD, a clinical instructor in the department of dentistry at the Icahn School of Medicine at Mount Sinai in New York City.
But recent research suggests that the relationship between oral health and arthritis is more complex than that, she notes. One 2008 study published in the Journal of Periodontology, for example, looked at 100 people — half with rheumatoid arthritis (RA) and half without. The study found that folks with RA were almost eight times more likely to have periodontitis, a risk that wasn’t explained by differences in oral hygiene alone.
A few years ago, Dr. Andrade and his colleagues at Johns Hopkins looked more deeply into the gum disease-arthritis connection and found striking similarities in the types of inflammatory proteins and immune antibodies that were present in both infected gums and in joints inflamed by rheumatoid arthritis.
“There is also good evidence to suggest that periodontal disease may happen before rheumatoid arthritis in some patients, and that has led to the hypothesis — and it’s still just a hypothesis — that maybe the arthritis doesn’t start in the joints, but may start some other place like the gums and spread from there.”
A small 2013 study in the journal Inflammation also found that people with psoriatic arthritis (PsA) were more likely to have severe periodontitis than people without PsA. Other types of arthritis are associated with oral health complications, too.
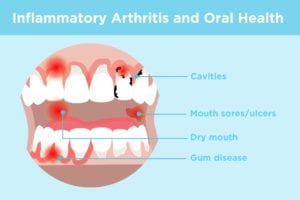
Common Oral Health Issues in People with Arthritis
Mouth sores (also called ulcers)
One 2019 study by researchers from the UK and Canada found that people with ankylosing spondylitis (AS) — a type of inflammatory arthritis that affects the spine and pelvis — were significantly more likely to have mouth sores than those without ankylosing spondylitis. Other inflammatory conditions such as reactive arthritis, Behçet’s disease, and systemic lupus erythematosus are associated with mouth sores, too. Oral ulcers can also be a side effect of medications like NSAIDS, immunosuppressive therapies, and methotrexate.
Dry mouth
Dry mouth and dry eyes are two of the main symptoms of Sjögren’s syndrome, an autoimmune condition in which a person’s immune system attacks the glands that produce saliva and tears. Some people with RA — and other autoimmune conditions such as lupus — also experience symptoms of Sjögren’s, says Dr. Andrade, and in these cases, they’re said to have “secondary Sjögren’s.” Dry mouth from primary or secondary Sjögren’s can cause pain, trouble swallowing, and changes in the way food and drinks taste.
Cavities
Saliva plays an important role in preventing cavities by protecting enamel from bacterial acids, so a reduced salivary flow due to Sjögren’s also increases the risk of tooth decay and cavities, explains Dr. Levi.
Gum disease
Bacteria in the mouth can stick to your teeth and over time become calcified into a hard substance known as calculus, explains Dr. Levi. Over time this calculus can lead to gum inflammation and irritation. If not interrupted with good hygiene and dental cleanings, this can lead to periodontitis, with bone loss and eventually tooth loss, she says.
Taking Care of Your Oral Health with Arthritis
Because some types of arthritis increase the risk of oral health issues, it’s important to establish good home hygiene habits, and a regular schedule of dental care at the dentist office. Here’s what to aim for:
Follow a regular cleaning routine. Brush twice a day for two minutes, and floss once a day. If arthritis in your wrists or hands makes gripping a toothbrush or twirling floss around your fingers uncomfortable, Dr. Levi suggests using small pre-threaded flossers — “they’re a little bit easier to use,” she says — and an electric toothbrush. “Using a toothbrush with a wider handle is more ergonomic.”
Use the right toothpaste. If you have dry mouth symptoms in addition to arthritis, experts at the Johns Hopkings Sjögren’s Center recommend avoiding whitening or abrasive toothpastes, and choosing a brand with fluoride that is especially labeled for “dry mouth.” A 0.05% sodium fluoride mouth rinse before going to bed can also help reduce the risk of cavities.
See your dentist at least once a year. The American Dental Association recommends “regular” dental visits. Generally that means twice a year and more frequently if your dentist or hygienist recommends it, says Dr. Levi. “Every patient is different, but as a general rule, it’s often recommended that patients receive cleanings and exams twice a year. If they have periodontal disease, it is often recommended that patients are seen more regularly,” she says.
Don’t ignore signs of infection. If you’re on immunosuppressive medications to help control your arthritis symptoms, you may be at an increased risk of bacterial and fungal infections of the mouth. So be sure to call your doctor or dentist if you have swelling in your mouth or on your gums, fever, swollen lymph nodes around your jaw, or a white coating on your tongue or inside of your cheeks, says Dr. Andrade.
Address gum disease if you have it. During an exam, your dentist will, among other things, look for signs of gingivitis, an inflammation of the gums that causes puffiness, redness, and bleeding that can lead to periodontitis if not addressed. She’ll also check the depth of the gum “pockets” around your teeth. Treatments for gum disease may include deep dental cleanings known as scaling or root planing, more frequent dental cleanings, and antibiotics applied directly to the gum pockets, says Dr. Levi. If your periodontitis is severe, or doesn’t respond to these treatments, your dentist may refer you to a gum specialist called a periodontist for surgery or other advanced remedies.