Have you been diagnosed with irritable bowel syndrome (IBS) but find that treatments aren’t helping? It’s possible that what you’re experiencing might be related to a condition called immunoglobulin G4-related disease (IgG4-RD).
While IBS and IgG4-RD can cause similar symptoms, especially in the digestive system, they are different conditions with unique causes and manifestations. Learn to recognize important warning signs, understand the essential diagnostic steps, and ask questions of your health care provider to ensure you receive the best possible care.
One patient, Charlotte Pilcic, is currently undergoing assessments to determine an accurate diagnosis for her ongoing pain and pancreatic mass related to suspected IgG4-RD. She described her experience with the testing process:
“I saw a gastroenterologist, and he did an endoscopic retrograde cholangiopancreatography (ERCP), and, I think, three endoscopic ultrasounds,” Charlotte recalls. “I had three negative biopsies. A stent was put in and caused me a lot of cramping and pain, and it was removed later. After three months of prednisone, the mass disappeared.”
Charlotte’s story offers insight into the types of testing patients undergo and highlights the challenges of diagnosing complex conditions. Let’s explore how IBS and IgG4-RD compare and differ.
What Is IgG4-RD?
IgG4-RD is an immune-mediated condition characterized by inflammation and scar tissue formation (fibrosis). It often presents as mass-like growths in various organs, such as the pancreas, retroperitoneal space, salivary glands, and kidneys. Because IgG4-RD can closely resemble other conditions like IBS, patients may sometimes receive unnecessary treatments—or even undergo surgeries—before getting the correct diagnosis.
A key indicator of IgG4-RD can be an elevated level of a specific antibody, IgG4, in the blood. Additionally, affected tissues typically show an increased number of IgG4-positive plasma cells. To diagnose this condition, doctors usually perform a blood test to measure IgG4 levels and may also conduct a biopsy of the affected area.
New treatments in development, and clinical trials are underway to find safer and more effective options for managing IgG4-RD.
Currently, steroids are the first-line therapy, but long-term use can lead to side effects such as weight gain, osteoporosis, high blood pressure, and diabetes. To mitigate these issues, healthcare providers may use steroid-sparing medications like DMARDs or rituximab—a targeted anti-CD20 therapy—to suppress the immune response and reduce the size of the mass-like lesions.
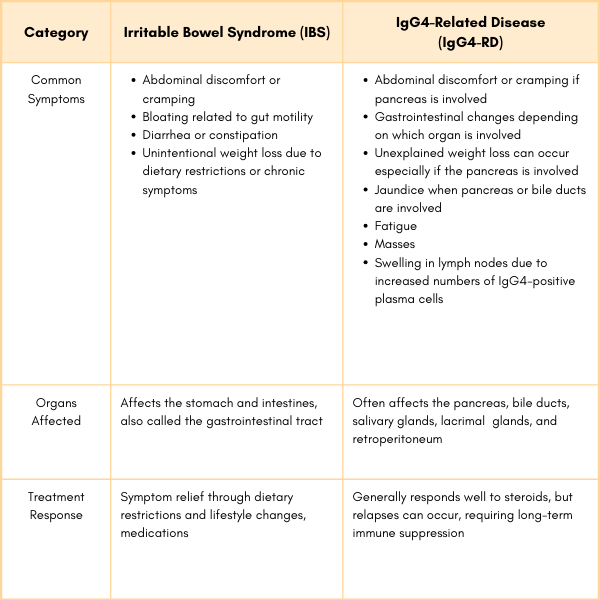
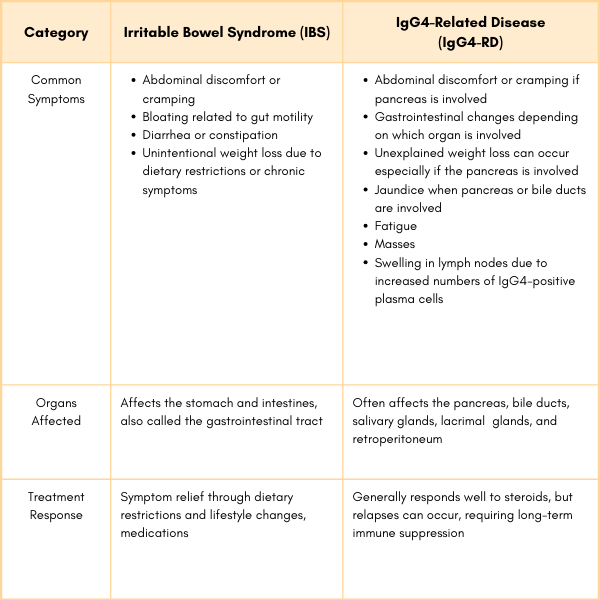
Comparing IBS and IgG4-Related Disease
IBS and IgG4-RD can affect digestion but stem from different underlying issues. Here’s how their key symptoms compare:
- Abdominal Pain – Both can cause pain, but IBS pain is linked to bowel movements, while IgG4-RD pain may come from organ inflammation – especially when the pancreas is affected.
- Bloating – IBS bloating is due to gut motility issues, whereas IgG4-RD bloating may result from inflammation.
- Diarrhea or Constipation – IBS symptoms vary by type (IBS-D, IBS-C, IBS-M), while IgG4-RD can lead to changes in bowel habits depending on which organs are involved.
- Weight Loss – IBS-related weight loss is often due to dietary changes or chronic symptoms, while in IgG4-RD, it’s typically caused by systemic inflammation or organ dysfunction.
Why is IgG4 Often Misdiagnosed as IBS?
Although some gastrointestinal symptoms overlap, IBS is a functional disorder without structural abnormalities, while IgG4-RD is an inflammatory condition with distinct systemic and histological features. Accurate diagnosis involves comprehensive testing and clinical evaluation.
Here’s why this misdiagnosis can occur:
- Overlapping Symptoms: Both conditions can present nonspecific gastrointestinal symptoms, such as abdominal pain, bloating, diarrhea or constipation, and nausea. These shared symptoms can make it challenging to distinguish between functional (IBS) and structural/inflammatory (IgG4-RD) disorders without further testing.
- Lack of Awareness of IgG4-RD: IgG4-related disease is less known and may not be immediately considered by clinicians, especially in patients presenting with common GI symptoms. IgG4-RD can involve multiple organs (e.g., pancreas, bile ducts, gastrointestinal tract), and its systemic nature might not be apparent initially.
- Minimal Initial Testing in IBS Diagnosis: IBS is a diagnosis of exclusion, meaning it is often diagnosed when other conditions are ruled out. The standard diagnostic workup for IBS often includes routine blood tests, stool tests, and imaging studies that may not detect IgG4-related disease unless specifically looked for. If IgG4-related disease is not specifically tested for, it might be missed and attributed to IBS.
- Masked by Food-Related Symptoms: Some studies suggest food sensitivities (e.g., IgG4 antibodies to certain foods) might play a role in IBS. This overlap in focus can lead to confusion, with IgG4-RD being overlooked when the presence of IgG4 is attributed to IBS.
Getting the Right Diagnosis
If you feel like standard IBS treatments aren’t working or something doesn’t feel right, it’s time to dig deeper. Here are steps to help you get a clearer diagnosis:
- Track your symptoms. Note when symptoms occur, how long they last, and any possible triggers (like food, stress, or illness). Tracking patterns—such as changes in pain, bloating, bowel habits, or weight—can make pinpointing the cause easier and rule out other conditions.
- Share your medical history. If possible, send your test results to your doctor before your appointment to maximize time discussing the next steps. Talk about your symptoms in detail—when they began, how severe they are, and if anything seems to trigger them. Don’t forget to mention any family history of autoimmune diseases!
- Ask about blood tests. Request a test for serum IgG4 levels, which may help differentiate IgG4-RD from IBS. Elevated levels might indicate IgG4-RD, although they aren’t definitively conclusive.
- Consider imaging studies. If you’re experiencing gastrointestinal symptoms, you may need an endoscopy or colonoscopy. Imaging options like CT or MRI scans should also be discussed to check if other organs are involved.
- Ask about a biopsy. Taking a tissue sample can sometimes provide essential information to confirm a diagnosis.
Questions to Ask Your Doctor
Your voice is important in your healthcare journey. Here are some key questions to bring to your appointment:
Could my symptoms be caused by something other than IBS, such as IgG4-related disease?
Have my imaging or blood tests shown anything that might suggest this condition?
Can we test my IgG4 antibody levels?
Should we consider a biopsy to confirm or rule out other conditions?
Should I see a rheumatologist or another specialist to rule out other conditions?
What are the next steps if my symptoms don’t improve with standard treatments?
Partnering with Your Doctor to Get Answers
Navigating the diagnosis of IgG4-related disease can feel overwhelming, but remember, you’re not in this alone. You play a crucial role in collaborating with your doctor to find the answers you seek. Here’s how you can take charge of your health in a supportive and productive manner:
Tips for Working with Your Doctor:
- Be bold and persistent. Your health is important! Don’t hesitate to speak up if you feel that treatments aren’t making a difference. It’s perfectly okay to ask for additional tests or even seek a second opinion. Your concerns matter, and it’s essential to advocate for your well-being.
- Keep a symptom journal. Documenting your symptoms can significantly aid your diagnosis. Note when your symptoms occur, how intense they are, and any potential triggers you notice. This information can provide valuable insights for your doctor, helping them better understand your condition.
- Consider a specialist. If you haven’t already, think about consulting a rheumatologist. These specialists focus on autoimmune diseases and can bring a wealth of knowledge and expertise to your situation. A specialist can help refine your diagnosis and tailor a treatment plan that suits your needs.
Remember, you are your own best advocate. Building a strong partnership with your doctor can help you better understand and manage your health. Don’t hesitate to express your feelings and concerns; your voice is crucial to this process. Together, you can work towards getting the answers and care you deserve.
Learn More About IgG4-RD
Click here to get more information on IgG4-RD including a guide to getting diagnosed, managing symptoms, and treatment options.
This article was made possible with support from Amgen.
Chen, L., Mattman, A., et al. Igg4-Related Disease: What a Hematologist Needs to Know. Haematologica. 2019. Doi: https://doi.org/10.3324/haematol.2018.205526.
Lee HS, Lee KJ. Alterations of Food-specific Serum IgG4 Titers to Common Food Antigens in Patients with Irritable Bowel Syndrome. J Neurogastroenterol Motil. 2017. Doi: https://doi.org/10.5056/jnm17054.
Ligaarden SC, Lydersen S, Farup PG. IgG and IgG4 Antibodies in Subjects with Irritable Bowel Syndrome: A Case Control Study in the General Population. BMC Gastroenterology. 2012. Doi: https://doi.org/10.1186/1471-230X-12-166.
Löhr, J-M., Beuers, U., Vujasinovic, M., et al. European Guideline on IgG4-Related Digestive Disease – UEG and SGF Evidence-Based Recommendations. United European Gastroenterology Journal. 2020. Doi: https://doi.org/10.1177/2050640620934911.
Zhang, X., Jin, X., Guan, L., et al. IgG4-Related Disease With Gastrointestinal Involvement: Case Reports and Literature Review. Frontiers in Immunology. 2022. Doi: https://doi.org/10.3389/fimmu.2022.816830.





