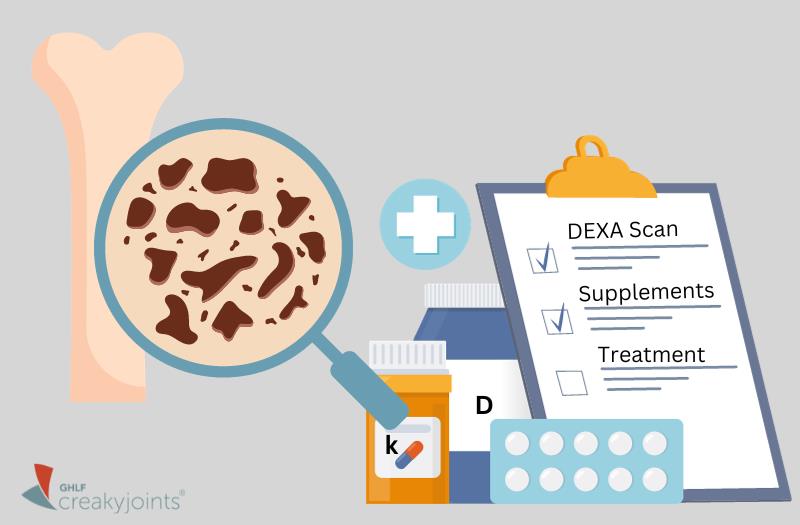
“Osteoporosis is a silent disease — until it’s not,” says endocrinologist Jessica Rachel Starr, MD, an Assistant Attending Physician at Hospital for Special Surgery. She explains that osteoporosis just means that the natural holes or pores in our bone are bigger than they should be on a bone density test.
“When they get bigger beyond a certain pre-defined score, we call it osteopenia,” says Dr. Starr. “And when it gets even bigger than that, we call it osteoporosis. But just having those holes in the bone and having them be large is painless.”
But here’s the thing: even if you don’t feel it now, the risks are real. When these holes or pores get bigger, your bones get more fragile, your muscle mass diminishes, and your risk of falls and fractures increases.
While osteoporosis alone isn’t life-threatening, it can result in significant fractures, leading to premature death in approximately 20 percent to 40 percent of affected individuals following an injury.
The good news: understanding osteoporosis, its treatments, and methods of prevention can ensure healthier bones and a more resilient skeletal system.
Understanding Osteoporosis and Healthy Bones
Our bones are dynamic structures, continuously breaking down and rebuilding. “Our body is constantly remodeling, even as adults we’re always building bone and breaking bone down,” says Dr. Starr.
However, when there’s an imbalance in the process — more bone being lost than being built — conditions like osteoporosis can develop. This imbalance can be influenced by numerous factors, including aging, a low body weight, decreased levels of sex hormones, smoking, and the use of certain medications like corticosteroids.
Ensuring strong bones requires attention at all stage of life. Osteoporosis isn’t just an issue confined to older individuals. An increasing number of people in their 20s, 30s, and 40s are receiving diagnoses.
While immediate medical treatment may not be necessary for every diagnosis, especially in younger, fit individuals with milder forms of osteoporosis, it’s essential to engage in an open conversation with healthcare providers about steps to fortify bones and prevent fractures.
“Doing something is better than doing nothing,” says Dr. Starr. “If someone promises me they’ll attend physical therapy for strength training and take some calcium, it’s still a step forward from when I first met them at the door where they weren’t doing those things.”
Treatment Options for Osteoporosis
If you and your provider decision on osteoporosis medication, there are several options, including:
- Anabolic agents: These medications stimulate bone formation and are recommended for those with severe osteoporosis.
- Anti-resorptive drugs: These medications prevent bone loss by blocking the action of osteoclasts, cells that break down bone tissue.
- Bisphosphonates: This group of drugs is the primary treatment for osteoporosis. They’re available as oral pills or IV infusions and work by reducing bone loss and enhancing bone density. Options include Actonel (risedronate), Boniva (ibandronate), Fosamax (alendronate), and Reclast (zoledronic acid).
- Calcitonin: These medications contain calcitonin, a hormone that boosts bone density, reduces the risk of spinal fractures, and alleviates fracture-related pain. Choices include Calcimar (an injection), as well as Fortical and Miacalcin (both nasal sprays).
- Hormone therapy: Though not recommended as a preventive or treatment measure for osteoporosis in menopausal women, hormone therapy can bolster bone health in women taking it for menopausal symptom relief. It’s also suitable for premenopausal women whose ovaries don’t produce adequate estrogen.
- Parathyroid hormone (PTH): This treatment involves hormones that promote bone formation and reduce bone resorption. Options, such as Forteo (teriparatide) and Tymlos (abaloparatide), are often prescribed for individuals with a high fracture risk, those who haven’t responded to other osteoporosis treatments, or those who’ve experienced side effects from other medications.
- Parathyroid (PTH1) agonists: These drugs increase bone formation and decrease bone resorption. Choices include Prolia (denosumab) and Xgeva (denosumab), both injectable medications designed for individuals at fracture risk or those with advanced breast cancer, respectively.
- Selective estrogen receptor modulators (SERMS): This category comprises one medication, Evista (raloxifene). It has bone-protective, estrogen-like effects without the associated risks of hormone replacement therapy (HRT), which isn’t used to treat osteoporosis anymore.
- Sclerostin inhibitors: This newer treatment is available for postmenopausal women diagnosed with osteoporosis and at high fracture risk. Evenity (romosozumab) mainly promotes bone formation and also aids in reducing resorption.
Supplements and Dietary Choices for Bone Strength
Diet plays an instrumental role in ensuring bone health, with certain foods naturally rich in bone-boosting nutrients. Daily intake of calcium and vitamin D are also important as they are crucial for building strong bones earlier in life and preserving bone strength as we age.
Why Calcium
An essential mineral, calcium has been clinically proven to improve bone density at the spine and the hip, says Dr. Starr. However, humans aren’t efficient at absorbing calcium, so in addition to a supplement, it’s importance to incorporate calcium-rich foods into your diet. Sources include dairy products, kale, bok choy, sardines, tuna, chia seeds, sweet potatoes, and figs.
The Role of Vitamin D
This nutrient helps aid calcium absorption. “If you have vitamin D deficiency, it will be very hard for the body to effectively absorb the calcium,” says Dr. Starr. “And if your vitamin D gets low enough and you can’t absorb the calcium, your body will start breaking down the bone to put more calcium into the blood.”
Other Supplements
“There’s a lot out there about boron, magnesium, and vitamin K,” says Dr. Starr. “But there isn’t good randomized controlled trial evidence where I would feel comfortable saying to people, yes, go out there and buy this.”
When shopping for supplements, Dr. Starr stresses opting for products with the United States Pharmacopoeia (USP) seal, which ensures quality, purity, and safe manufacturing processes. Before starting any supplement, consult with a health care professional to ensure it’s right for you and does not interfere with any other medication you are taking.
The main takeaway: Good bone health is about more than just medicine. It means understanding your body, getting the right nutrients, staying active, and talking with your doctor to ensure proper screening and the appropriate treatment for your age and stage.
Learn more about what you can do to prevent fractures and strengthen your bones at StrongBonesAndMe.org.
This article was made possible with support from Amgen.
Bone Health & Osteoporosis Foundation. Nutrition. https://www.bonehealthandosteoporosis.org/patients/treatment/nutrition/.
Guzon-Illescas O, Perez Fernandez E, Crespí Villarias N, et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res. 2019;14:203. doi: https://doi.org/10.1186%2Fs13018-019-1226-6.
Interview with Endocrinologist Jessica Rachel Starr, MD, an Assistant Attending Physician at Hospital for Special Surgery .