If your lower back or butt hurts when you get up from a chair or climb a set of stairs, your sacroiliac (SI) joints may be to blame. In fact, research suggests the SI joint is the source of pain in 15 to 30 percent of people with chronic low back pain.
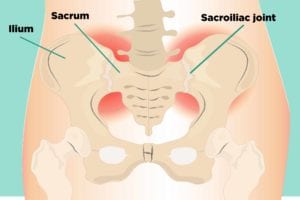
You have two SI joints in your lower back — one on each side of your spine. They connect the sacrum (base of your spine) to the ilium (the top part of your pelvis), with strong ligaments that hold them in place. Together, these joints support the weight of your upper body when you stand or walk, helping to absorb impact and reduce pressure on your spine.
Causes of Sacroiliac (SI) Joint Pain
Arthritis is one possibility. Axial spondyloarthritis [which includes ankylosing spondylitis (AS) and non-radiographic axial spondyloathritis (nr-AxSpA)] or psoriatic arthritis (PsA) can cause inflammation in the SI joint, as well as the vertebrae in your spine, which leads to pain and stiffness in your lower back and hips. Osteoarthritis, which occurs when the cartilage that cushions and protects the ends of your bones gradually deteriorates, may affect the SI joint’s cartilage and cause pain.
Other conditions that lead to sacroiliac pain include:
- Trauma: A sudden impact, such as a fall car accident, can damage the SI joint.
- Pregnancy: Hormones are released to loosen ligaments and joints to prepare for childbirth, which changes the way the SI joint moves and makes it less stable. Extra weight also puts more stress on the SI joints, leading to additional wear.
- Abnormal walking pattern: If one leg is shorter than the other, or you favor one leg when you walk because of pain, it can lead to SI joint pain.
- Spine surgeries: Fusing vertebrae reduces flexibility in the spine, which can increase stress on the SI joint.
- Infection: In rare cases, the SI joint can become infected and degenerate.
What SI Joint Pain Feels Like
For some, SI joint pain could be dull and achy, for others it can be sharp and stabbing. You’re most likely to feel SI joint pain in your lower back and buttocks, but it can move out to your hips and down to your thighs, groin, and even your feet. You may also experience:
- Pain only one side of your lower back, or both sides
- Pain with prolonged standing
- Pain that worsens with walking, running, or taking large strides
- Pain that worsens with certain movements, such as getting up from a chair, climbing stairs, or turning in bed
- Muscle tightness and tenderness in your hips or buttocks
If your SI joint pain is due to inflammatory back pain such as from ankylosing spondylitis, there are other distinct features, such as pain that has lasted more than three months, feels better with movement and worse with rest, and often wakes you up in the middle of the night. Read more about inflammatory back pain vs. mechanical back pain, or take a quiz to see if your back pain could be inflammatory.
How SI Joint Pain Is Treated
Step one: Stop doing things that hurt your SI joints. Modify or avoid activities that worsen your pain to help reduce inflammation in the joint. Alternating ice and heat might help ease sacroiliac joint pain. Other ways to help find relief:
Medications
Depending on the cause of your SI joint pain, your doctor may recommend:
- Pain relievers (over-the-counter or prescription, if needed)
- Anti-inflammatory meds (such as nonsteroidal anti-inflammatory drugs, or NSAIDs)
- Muscle relaxants (to help reduce muscle spasms)
- Biologics, such as tumor necrosis factor (TNF) inhibitors or others (to treat axial spondyloarthritis or ankylosing spondylitis)
Physical therapy
Your doctor or physical therapist can tailor a program for you that may include:
- Massage therapy to ease sore muscles and improve mobility in the joint, hip, and low back
- Range-of-motion and stretching exercises to maintain joint flexibility
- Strengthening exercises to help stabilize the joint and reduce the stress load
- Body mechanics to teach you to how to move and use your body in everyday activities to ease SI joint dysfunction and pain
Non-surgical procedures
If you’re still hurting after conservation therapies, your doctor might suggest:
- Steroid shots: Cortisone can be injected directly into the SI joint to reduce inflammation and pain. Because it’s deeper within the body than most joints, the steroid injections are usually given in a hospital setting, under live X-ray guidance. You can get only a few joint injections a year because the steroids can weaken your joint’s bones and tendons.
- Radiofrequency ablation: This procedure uses radio waves to destroy the nerve fibers that carry pain signals in the joint, therefore reducing pain.
Surgery
If all other treatments don’t provide pain relief, your doctor may recommend joint fusion surgery — a minimally invasive procedure that uses metal hardware to join the two bones in the SI joint together so they fuse.
Keep Reading
If you enjoyed reading this article, you’ll love what our video has to offer.