Here’s the thing: not only *should* you stay active when you have osteoporosis, but your bones kind of need you to. Osteoporosis is a condition where the body loses too much or makes too little bone tissue, which leaves your bones brittle, weak, and more likely to break. And if you have inflammatory arthritis, your chance of developing osteoporosis may increase.
As counterintuitive as it may seem, certain types of exercise can actually help prevent and manage osteoporosis. Low-impact weight-bearing exercises (such as walking) help build bones and keep them strong, according to the National Osteoporosis Foundation (NOF). Muscle-strengthening exercises have the same benefit: using free weights, elastic bands, or your own body weight strengthens muscles and helps maintain bone density. Read more about good osteoporosis exercises that help keep bones strong.
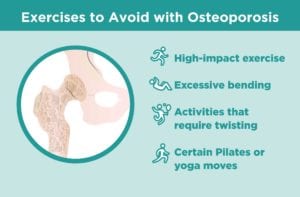
But not all exercises are safe or recommended for people with osteoporosis. The reason: Certain activities and moves can increase your risk of fracture, says Karen Kemmis, PT, DPT, physical therapist in New York who works with the National Osteoporosis Foundation (NOF).
Some high-impact activities may put too much force on relatively weak bones. Sports that are associated with a high risk of falls are also a no-no. Other activities to avoid: exercises where you need to bend forward and twist your waist, which can raise the risk of compression fractures in your spine.
You should always talk to your health care provider about which types of exercise are best and safe for you, and which ones you should not do or at least modify.
Avoid: High-Impact Exercises
Here is more information on specific activities that you should likely avoid if you have low bone density or osteoporosis.
Running
Weight-bearing aerobic activities strengthen and slow bone loss in your legs, hips and lower spine. And when you pound the pavement on a jog or run, it increases the stress on your bones to provide more strengthening benefits. But if your bones are weak from osteoporosis, something as high impact as running can lead to injury or fracture. Power walking and walking briskly are much safer and almost as effective, according to the NOF.
Jumping
Think jumping rope, jumping jacks, or any other exercises that involves that abrupt and explosive loading or impact when your feet hit the floor. Avoid jerky, quick movements as well, suggest experts at the Mayo Clinic; instead choose exercises with slow, controlled movements.
Avoid: Excessive Bending and Twisting
Sit-ups and Toe Touches
Both of these exercises involve bending forward, which puts stress on the joints in your spine, or vertebrae. “The front of each vertebrae is always weaker, whether you have osteoporosis or not,” says Kemmis. If your bones are healthy, that portion is still less dense, but the vertebrae is strong enough to tolerate the forward movement, she explains. “If you have low bone density, however, and you put a lot of force or pressure into the front of the spine — such as in a sit-up or toe touch — it increases your risk of a compression fracture.” Once you have one compression fracture, it can trigger a “cascade of fractures” in the spine, says Kemmis.
Compression fractures may cause back pain, but they often don’t cause any symptoms. Take a PainSpot assessment to see if your back pain could be due to an osteoporosis-related compression fracture.
Certain Yoga and Pilates Poses
Both yoga and Pilates are good in that they improve strength, balance, and flexibility, which can all help with preventing falls. But some poses or movements can strain the spine and put fragile bones at risk for fracture. With low bone density or osteoporosis, you should avoid:
- Rounding poses or rounded spine movements
- Spine twist or any deep twists
- Corkscrew or bicycle
- Deep hip stretches (like the pigeon pose)
- Warrior pose
- Overpressure from teachers
Some yoga and Pilates movements can be safe, such as the tree pose or plank. A physical therapist can help recommend or modify moves that are safe and appropriate for you.
Golf and Tennis
That forceful twist at the waist when you swing a club or racket can put extra force on the joints and discs in your spine, which may result in fracture. Imagine if you’re behind the wheel of your car, trying to back out of a parking spot, explains Kemmis. You’re twisting around, looking over your shoulder to get a good view. “At some point, the muscles and ligaments are pulled to the end of their stretch,” she says. “If you force it further, the bone has the take the strain. If the bone is weak, it may not tolerate the strain.” The same is true for golf and tennis: If you rotate to the very end of your range of motion, it could put your bones at risk, she says. A case study found three women with osteoporosis sustained compression fractures in their spine during mid-swing while golfing.
Avoid: Activities with a High Risk of Falling
Skiing and Other High-Fall Risk Sports
Hitting the slopes comes with a high risk of falls — and falls are how the majority of fractures occur, says Kemmis. Some other activities on that list: ice skating, rollerblading, and any contact sport, adds Kemmis.
Should Everyone with Osteoporosis Avoid All of These Exercises?
Not necessarily. Exactly how much impact is unsafe or which activities should always be avoided depends on your history of fractures, severity of your osteoporosis, and overall health. “If someone has had a fracture in the spine without major trauma, it’s important to be very conservative with exercise,” advises Kemmis. But if you’re generally fit and strong despite having osteoporosis, you might be able to engage in somewhat higher-impact exercise than can someone who is frail.
There’s no one-size-fits-all prescription for exercise. If you’re not sure how healthy your bones are, talk to your doctor. Your provider or physical therapist can help determine the safest activities for you.