Check out A Patient’s Guide to Understanding Rheumatoid Arthritis and Heart Disease for more information on this topic.
If you have rheumatoid arthritis (RA), the same inflammation that affects your joints can take a toll on the rest of your body — including your heart and blood vessels. In fact, people with RA are nearly 50 percent more likely than the general population to develop cardiovascular disease and 50 percent more likely to die from it.
While that sounds frightening, the truth is not everyone with rheumatoid arthritis has the same heart risks. Determining where you fall on the risk spectrum — and acting accordingly to protect your heart — is key to staying healthy.
“It is critical to assess traditional cardiovascular risks in every RA patient, as these risk factors contribute to cardiovascular events [like strokes and heart attacks] in people with RA,” says UCLA rheumatologist Christina Charles-Schoeman, MD. “Does the patient have high blood pressure? Do they smoke? Do they have diabetes? Do they exercise?”
These and other traditional risk factors — combined with some that are unique to RA — need to be regularly assessed, yet such evaluations often fall through the cracks.
Part of the problem is that many rheumatoid arthritis patients only see a rheumatologist, yet rheumatologists often assume that managing cardiovascular issues are the domain of an internist or cardiologist.
“A large number of RA patients don’t even get a cholesterol test,” says rheumatologist Iris Navarro-Millan, MD, Assistant Professor of Medicine at Weill Cornell Medical College and Assistant Attending Physician at Hospital for Special Surgery in New York City. While your cholesterol is just one piece of the heart-health puzzle, patients who are missing this most basic metric are not likely to be having more in-depth discussions about heart disease with their health care providers, she adds.
Who is actually in charge of your heart health? In a word: you. Make it your job to see your internist at least annually and talk to your rheumatologist about cardiovascular disease so that you get the tests you need to know your heart disease risk factors and keep your cardiovascular system healthy.
And you can use these tips to reduce your risk of heart disease when you have rheumatoid arthritis.
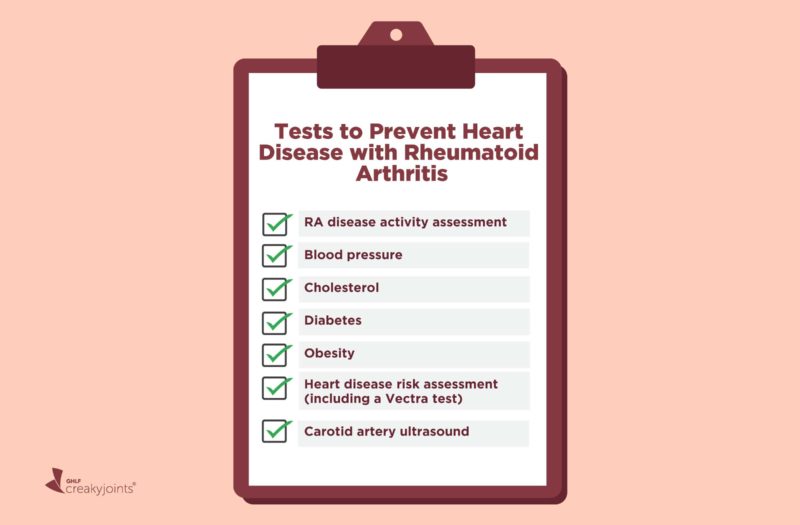
The Basics: Tests Everyone with Rheumatoid Arthritis Needs
RA disease activity assessment
Keeping your rheumatoid arthritis well-controlled is one of the best things you can do for your joints and your heart. According to a study published in the journal Arthritis & Rheumatology, people whose RA was in remission were 53 percent less likely to experience a serious cardiovascular event during the study’s three-year follow-up period.
Your rheumatologist should be assessing your RA disease activity at least once a year using a scoring tool that is approved by the American College of Rheumatology. There are many different ways to measure RA disease activity, but each involves different combinations of assessing factors like counts of painful and swollen joints, blood tests for inflammatory markers, and patients’ and physicians’ reports of pain and function in everyday life. They include:
- Clinical Disease Activity Index (CDAI)
- Simple Disease Activity Index (SDAI)
- Routine Assessment of Patient Index Data (RAPID3)
- 28-Joint Disease Activity Score (DAS28)
- Patient Activity Scale II (PAS-II)
- Vectra Multibiomarker Disease Activity (MBDA) score
Meanwhile, your rheumatologist should be taking note of whether you have other RA-related issues that could spell trouble for your joints and your heart: Extra-articular problems (such as rheumatoid nodules, eye inflammation, or gastrointestinal problems) could spell trouble for your cardiovascular system. They indicate more advanced disease and have been linked to developing atherosclerosis, which meanis plaque builds up in your arteries and narrows and hardens them.
You should also talk to your rheumatologist about how your medications might be impacting your cardiovascular health. Some RA medications may increase the risk for potential heart problems. Glucocorticoids like prednisone tend to be the most problematic, especially when taken in high doses for a long time.
Blood pressure test
Blood pressure should be measured every time you see any health care provider. Ideally, your blood pressure should be less than 120/80 mm Hg. Hypertension (chronic high blood pressure), is one of the biggest risk factors for stroke, heart attack, and other serious cardiovascular events. Studies have shown that RA patients are more likely than the general population to have hypertension, though scientists are still trying to figure out why.
Cholesterol test
Cholesterol is a fatty substance in the blood that can accumulate in your arteries and restrict or block blood flow. According to the American Heart Association, adults at normal risk for cardiovascular disease should have a fasting lipoprotein panel (a blood tests that measures different types of cholesterol) every four to six years, but those at higher risk for heart disease should get checked more often. Ask your internist and rheumatologist what they recommend. Once a year might be advisable, especially if you have other heart disease risk factors (such as obesity, family history, or high RA disease activity).
Your doctor might also want to test you more frequently if you’re taking certain RA medications (a JAK inhibitor or IL-6 inhibitor) because these drugs have the potential to raise cholesterol, says rheumatologist Christie Bartels, MD, Associate Professor at the University of Wisconsin in Madison.
JAK inhibitors include tofacitinib (Xeljanz), baricitinib (Olumiant), and upadacitinib (Rinvoq). IL-6 inhibitors include such as tocilizumab (Actemra) and sarilumb (Kevzara).
A lipoprotein panel should yield several numbers: total cholesterol, LDL cholesterol (the “bad” kind, which contributes to the buildup of plaque in your arteries), HDL cholesterol (the “good” kind, which helps remove LDL from your arteries), and triglycerides (another type of blood fat).
- Total cholesterol should ideally be less than 200 mg/dL
- LDL cholesterol should ideally be less than 100 mg/dL
- HDL cholesterol should ideally be 40 mg/dL or higher in men or 50 mg/dL or higher in women
- Triglycerides should ideally be less than 150 mg/dL
Diabetes test
You should have an A1C test, a blood test that provides an indication of your average blood glucose levels over the past three months, at least every three years starting at age 45. If your A1C is 6.5 percent or higher it means you have type 2 diabetes, which is a major risk factor for heart disease. An A1C between 5.7 and 6.5 percent is considered prediabetes. A1C lower than 5.7 percent is considered healthy.
Most people with diabetes should be taking a statin, a medication that reduces the risk of serious cardiovascular events by lowering cholesterol, reducing inflammation in the arteries, and stabilizing plaque so it’s less likely to break off and block blood flow.
Obesity assessment
Your health care provider should check your weight and calculate your body mass index (BMI) at every visit. At the very least, be sure to review it annually with your internist or rheumatologist. Generally speaking, people with a BMI that is considered overweight or obese face a higher risk of heart disease.
Maintaining a healthy BMI is also important for your RA. People with RA who are overweight or obese are less likely to be in remission.
Overall heart disease risk assessment
You can also ask your internist or rheumatologist about calculating your personal chances of having a serious cardiovascular event. The most common way to do this by using the American College of Cardiology (ACC)/American Heart Association (AHA) risk calculator, which takes into account your age, biological sex, weight, cholesterol, blood pressure, and smoking and diabetes status and makes a prediction about your chances of having a heart attack or stroke in the next 10 years.
Because having RA is an additional important heart disease risk factor, the European League Against Rheumatism (EULAR) advises taking the ACC/AHA risk score and multiplying it by 1.5.
How useful this multiplier is unclear, however, so it’s okay if your doctor decides to skip it. Even if your doctor doesn’t use it, they should keep in mind that someone who ends up on the threshold of being high risk per the ACC/AHA calculator probably ought to be bumped up as a result of having RA, says Dr. Bartels.
Additional Heart Tests Worth Considering
Vectra Cardiovascular Risk
This blood test was initially designed to assess overall inflammation and RA disease activity by looking at multiple different biomarkers that can help predict the risk of future disease progression and joint damage.
The test has recently been adjusted so that it also provides information about an RA patient’s chances of having a serious cardiovascular event over the next three years. The current version of the test, called Vectra Cardiovascular Risk, uses a few additional biomarkers from the original test along with clinical information about a patient (such as age, smoking status, and whether they have diabetes) so that all this information can be factored in.
Research presented at the 2020 meeting of the American College of Rheumatology found that this test accurately predicts cardiovascular event risk in RA patients, including in those who were already taking statins and those who had diabetes.
Rheumatologist Jeffrey Curtis, MD, MPH, a Professor of Medicine at the University of Alabama at Birmingham who has led several manufacturer-funded studies on Vectra, says he was interested in vetting the test because he believes that health care providers need an easy, practical way to gain insights about the cardiovascular health of their RA patients. Dr. Curtis hopes that doctors will use the information it yields to generate a conversation about a patient’s personal heart health risk and what to do about it.
Depending on what your doctor believes is driving your risk, you might be advised to start statin therapy, make specific lifestyle changes, tweak your RA medication regimen, or see a cardiologist for further testing.
Carotid artery ultrasound
Similar to getting an ultrasound during pregnancy, this non-invasive imaging test uses soundwaves to peek inside the carotid arteries in your neck. Blood from your heart flows through these arteries to your brain. If there is any narrowing or obstruction, it means you’re at a higher risk for having a stroke.
Most of the RA patients who participate in the RA cardiovascular disease program at UCLA have this test, says Dr. Charles-Schoeman. “Identifying the presence or absence of atherosclerotic plaque in the neck arteries has been useful in assessing [cardiovascular risk],” she says. “Patients also seem more aware and engaged in their cardiovascular health when they find out that they may have some plaque in their arteries.”
Heart Tests You Might Need If You’re at High Risk or Having Symptoms
Exercise stress test
This test involves walking on a treadmill while a doctor (usually a cardiologist) monitors your heart rate, breathing, blood pressure, and the electrical activity of your heart. It’s sometimes combined with an imaging test (nuclear stress test). With this version, you’ll be injected with a tracer dye so that cameras can watch to see if certain areas of your heart aren’t getting enough blood. This test could show that you have plaque buildup in your arteries or a heart rhythm problem, or it could be used to help monitor that a treatment or procedure you’ve had is working as it should be.
Electrocardiogram (EKG)
Small electrodes are attached to the skin on your chest, arms, and legs, then connected to a machine that measures electrical activity of your heart. An EKG could show signs of an irregular heartbeat, blocked arteries, heart failure, or other damage to the heart.
Echocardiogram (heart ultrasound)
As with an EKG, this test involves electrodes, but your provider will also use an ultrasound to see how blood is moving through your heart. This test provides information about how blood flows through the heart, so it can reveal things like damage to the heart muscle or issues with pumping strength due to heart failure.
Cardiac computed tomography (CT scan)
Another imaging test, this CT scan involves a special X-ray tube that rotates around you and takes pictures of your heart and chest as the machine moves. This technology can be used to measure levels of coronary calcium, which tells you about how much calcified plaque there is in your arteries. It can reveal things like plaque buildup in your arteries or heart valve problems.
Magnetic resonance imaging (cardiac MRI)
Instead of sound waves or X-rays, this test uses a magnetic field and radiofrequency waves to view the blood vessels in and around your heart. An MRI can tell your doctor about things like weakened/damaged heart muscle, heart valve disease, coronary artery disease, and heart failure.
Cardiac catherization and angiography
This test is most likely to be performed if your doctor suspects that you have a serious blockage. A thin catheter gets threaded through a vessel in your groin, arm, or neck and up through your heart. A contrast dye is put into the catheter and X-rays of the vessels are taken. If you have a blockage, your doctor might put in a coronary stent (which props open a constricted vessel) or perform an angioplasty (which involves inflating a tiny balloon that pushes plaque out of the way).
This article is part of A Patient’s Guide to Understanding Rheumatoid Arthritis and Heart Disease and was made possible with a grant from Myriad Genetics, Inc.
10 Heart Tests Your Doctor Might Order, and What They Mean. Michigan Health. February 3, 2020. https://healthblog.uofmhealth.org/heart-health/10-heart-tests-your-doctor-might-order-and-what-they-mean.
Agca R, et al. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Annals of the Rheumatic Diseases. January 2017. doi: http://dx.doi.org/10.1136/annrheumdis-2016-209775.
Assessing Your Weight and Health Risk. National Heart Lung and Blood Institute. U.S. National Institutes of Health. https://www.nhlbi.nih.gov/health/educational/lose_wt/risk.htm.
Avina-Zubieta JA, et al. Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis & Rheumatism. December 2008. doi: https://doi.org/10.1002/art.24092.
Avina-Zubieta JA, et al. Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies. Annals of the Rheumatic Diseases. September 2012. doi: http://dx.doi.org/10.1136/annrheumdis-2011-200726.
Beyond the coronary arteries: Possible benefits of statin drugs Part II: Specific syndromes. Harvard Men’s Health Watch. May 2011. https://www.health.harvard.edu/heart-health/beyond-the-coronary-arteries-possible-benefits-of-statin-drugs-part-ii-specific-syndromes.
Cardiac Catherization. American Heart Association. https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/cardiac-catheterization.
Cardiac Catherization. Johs Hopkins Medicine. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/cardiac-catheterization.
Carotid Ultrasound. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/carotid-ultrasound/about/pac-20393399.
Cholesterol Levels: What You Need to Know. Medline Plus. NIH National Library of Medicine. https://medlineplus.gov/cholesterollevelswhatyouneedtoknow.html.
Curtis JR, et al. Performance of the MBDA-based CVD Risk Score in RA Patient Groups of Clinical Interest. Arthritis & Rheumatology [abstract]. November 2020. https://acrabstracts.org/abstract/performance-of-the-mbda-based-cvd-risk-score-in-ra-patient-groups-of-clinical-interest.
Coronary artery disease. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/diagnosis-treatment/drc-20350619.
Do I Need a Coronary Calcium Score? Texas Heart Institute. https://www.texasheart.org/heart-health/womens-heart-health/straight-talk-newsletter/do-i-need-a-coronary-calcium-score.
Echocardiogram. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/echocardiogram/about/pac-20393856.
Electrocardiogram. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/electrocardiogram.
England BR, et al. 2019 Update of the American College of Rheumatology Recommended Rheumatoid Arthritis Disease Activity Measures. Arthritis Care & Research. December 2019. doi: https://doi.org/10.1002/acr.24042.
Exercise Stress Test. American Heart Association. https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/exercise-stress-test.
Heart-Health Screenings. American Heart Association. March 22, 2019. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/heart-health-screenings.
Heart Risk Calculator. http://www.cvriskcalculator.com.
Interview with Christie Bartels, MD, rheumatologist and Associate Professor at the University of Wisconsin in Madison
Interview with Christina Charles-Schoeman, MD, rheumatologist at UCLA Health in Los Angeles
Interview with Iris Navarro-Millan, MD, Assistant Professor of Medicine at Weill Cornell Medical College and Assistant Attending Physician at Hospital for Special Surgery in New York City
Interview with Jeffrey Curtis, MD, MPH, a rheumatologist and Professor of Medicine at the University of Alabama at Birmingham
Manavathongchai S, et al. Inflammation and Hypertension in Rheumatoid Arthritis. The Journal of Rheumatology. November 2013. doi: https://doi.org/10.3899/jrheum.130394.
Rheumatoid Arthritis (RA) Clinical Presentation. Medscape. February 7, 2020. https://emedicine.medscape.com/article/331715-clinical.
Sapundzhieva T, et al. Body Mass Index Impact on Disease Activity, Clinical and Sonographic Remission Rates in Patients with Rheumatoid Arthritis. Current Rheumatology Reviews. July 2019. doi: https://doi.org/10.2174/1573397115666181130143239.
Should you consider a coronary artery calcium scan? Harvard Health Letter. June 2014. https://www.health.harvard.edu/heart-health/should-you-consider-a-coronary-artery-calcium-scan-.
Solomon DH, et al. Disease Activity in Rheumatoid Arthritis and the Risk of Cardiovascular Events. Arthritis & Rheumatology. June 2015. doi: https://doi.org/10.1002/art.39098.
Zegkos T, et al. Cardiovascular risk in rheumatoid arthritis: assessment, management and next steps. Therapeutic Advances in Musculoskeletal Disease. June 2016. doi: https://doi.org/10.1177/1759720X16643340.