Diabetes is a disease that occurs when blood sugar, or blood glucose, levels rise higher than normal because of problems with the way your body produces the hormone insulin. Glucose is a main source of energy for the cells that make up your muscles and tissues. Too much sugar in your blood for too long, however, can lead to serious health problems.
There are two main types of diabetes: type 1 and type 2 — both of which can cause high blood sugar, but in different ways. Think of glucose as fuel that feeds your body’s cells. To be able to enter cells and produce energy, glucose needs insulin — a hormone made by the pancreas. If your body doesn’t make enough — or any — insulin, or doesn’t use insulin properly, glucose builds up in your blood and doesn’t reach your cells. If you have type 1 diabetes, your body doesn’t make insulin. With type 2 diabetes, your body either resists the effects of insulin, or doesn’t make enough of it to maintain normal glucose levels.
What does any of this have to with arthritis — a disease that affects your joints? A whole lot, actually.
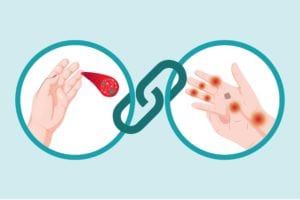
Studies have shown having inflammatory arthritis, like rheumatoid arthritis (RA), is related to an increased risk of both type 1 and type 2 diabetes. Psoriatic arthritis (PsA) and type 2 diabetes are also strongly linked. And osteoarthritis (OA) and type 2 diabetes often co-exist in older adults. In fact, nearly half of adults who have diabetes also have arthritis, according to research in the journal Diabetes Care.
Rheumatoid Arthritis and Type 1 Diabetes
Just like RA, type 1 diabetes is an autoimmune disease — which occurs when your immune system mistakenly attacks your body. In RA, the target is the synovial tissue that lines the joints, leading to pain, stiffness, swelling, and a host of other rheumatoid arthritis symptoms. With type 1 diabetes, the immune system destroys insulin-producing cells in the pancreas.
“If someone has one autoimmune disease, they are far more likely to have a second,” says Christopher Morris, MD a rheumatologist with Arthritis Associates of Kingsport, in Tennessee. In fact, research shows about 25 percent of people with one autoimmune disease later develop at least one more.
Data presented at the 2019 European Congress of Rheumatology annual meeting found people with RA were significantly more likely to also have type 1 diabetes (as well as inflammatory bowel disease) than those without RA. They were diagnosed with type 1 diabetes disease before developing RA, which suggests that type 1 diabetes may somehow predispose someone to later developing RA. Genetics may play a role. Studies show a gene called PTPN22 is linked to both RA and type 1 diabetes.
Inflammatory Arthritis and Type 2 Diabetes
Experts don’t know for sure how inflammatory arthritis such as RA and PsA are connected with diabetes, but research suggests certain factors may drive an association, including:
Inflammation: Both rheumatoid arthritis, psoriatic arthritis, and type 2 diabetes are characterized by inflammation, says Jessica Starr, MD, an endocrinologist at Hospital for Special Surgery in New York City. “There are studies that have shown that having RA increases your risk for developing type 2 diabetes and having type 2 diabetes increases your risk for developing RA,” says Dr. Starr. “A common mediator for this may be inflammation, but the data isn’t completely clear.”
What researchers do know is that having more inflammation — such as that occurs in rheumatoid arthritis, psoriatic arthritis, and other kinds of inflammatory arthritis — promotes insulin resistance, and could promote type 2 diabetes, says John Davis, III, MD, a clinical rheumatologist at the Mayo Clinic in Rochester, Minnesota. (Insulin resistance is an early stage of type 2 diabetes where the body becomes less able to use insulin efficiently.) Some of the same inflammatory markers that are high in people with inflammatory arthritis are also seen in people with diabetes.
Certain arthritis medications: Steroids such as prednisone are frequently prescribed for inflammatory arthritis patients to help reduce inflammation and slow joint damage. These corticosteroids are known for having potentially serious side effects, especially when used for long periods of time or at high doses. One such side effect is an increased risk for type 2 diabetes. “Steroids impair the body’s ability to synthesize and release insulin to process the carbohydrates in the food we eat,” explains Dr. Starr.
Inactivity: People with inflammatory arthritis may avoid exercising because of their fatigue and achy, stiff joints. (Read more here about why it’s a huge myth that you shouldn’t exercise with arthritis.) The less active you are, the greater your risk of developing type 2 diabetes. Immobility can worsen insulin resistance and predispose you to weight gain, says Dr. Starr. Being overweight or obese is a main risk factor for type 2 diabetes. Being overweight also can make it harder to manage your inflammatory arthritis.
Osteoarthritis and Type 2 Diabetes
People with type 2 diabetes are more susceptible to developing OA. Research suggests part of the reason may be obesity and aging, which are shared risk factors for both conditions.
More recently, research has found that high blood sugar may have a direct impact on cartilage and bone health, due in part to harmful compounds called advanced glycation end products (AGEs). They form in your bloodstream when protein or fat combine with sugar. Your body naturally rids itself of the compounds, but if you have high blood sugar, you’re at a higher risk of producing too many AGEs too quickly, which can build up in the body. “The accumulation of AGEs can damage many tissues, including bone and cartilage,” says Dr. Starr. High levels of AGEs can also lead to inflammation, she adds.
Warning Signs of Diabetes
Though type 1 diabetes usually first appears during childhood or adolescence, it can also develop in adults. Type 2 diabetes is the far more common type, and can develop at any age. It occurs most often in middle-aged or older people.
Type 2 Diabetes
Signs and symptoms usually develop very slowly, over several years, and can include:
- Increased thirst and urination
- Increased hunger
- Fatigue
- Blurred vision
- Unintended weight loss
- Sores that don’t heal
Type 1 Diabetes
Signs and symptoms can happen relatively quickly, and can include:
- Increased thirst and frequent urination
- Extreme hunger
- Weakness
- Blurred vision
- Unintended weight loss
How to Reduce Your Risk of Diabetes When You Have Arthritis
There’s no way to prevent type 1 diabetes. But there are steps you can take to reduce blood sugar and lower your chances of developing type 2 diabetes, such as:
Stick to your arthritis treatment plan
Keeping your disease activity under control can help reduce inflammation in your body. Some arthritis medications have been shown to protect against diabetes. Research published in the journal Arthritis Care and Research found RA patients who were given a class of drugs called TNF-alpha inhibitors — such as etanercept (Enbrel) and adalimumab (Humira) — were 51 percent less likely to develop diabetes, compared to those who didn’t. If you’re concerned about your type 2 diabetes risk (say, because of a family history or other risk factors), ask your doctor about which arthritis medications may be better for you.
Be more active
Get at least 30 minutes of physical activity, such as walking, at least five days a week. Exercise helps you control your weight and reduces blood glucose levels, as well as reduces arthritis pain and improves function. Talk to your doctor to determine which exercises are safest for you.
Shed extra pounds
If you’re overweight, losing 5 to 7 percent of your body weight can reduce your risk of diabetes. For a 200-pound person, that’s a 10- to 14-pound weight loss.
Eat healthy
Focus your diet on fruits, vegetables, whole grains, low-fat dairy, and lean sources of protein, including beans, nuts, fish, and lean cuts of meat. Control your portions to help cut calories, and choose foods that are lower in fat and higher in filling fiber.