Check out “Your Guide to Precision and Personalized Medicine for Rheumatoid Arthritis” for more information on this topic.
Precision medicine offers a wealth of potential for those living with rheumatic disease and other conditions. It goes beyond the traditional one-size-fits-all approach to treatment and instead takes into account your genes, lifestyle, and environment, per the National Institutes of Health (NIH).
However, misconceptions about this field could prevent individuals like you from getting the best treatment for your condition. In fact, even your doctor may not know much about precision medicine, which means knowledge and self-advocacy are your most valuable tools.
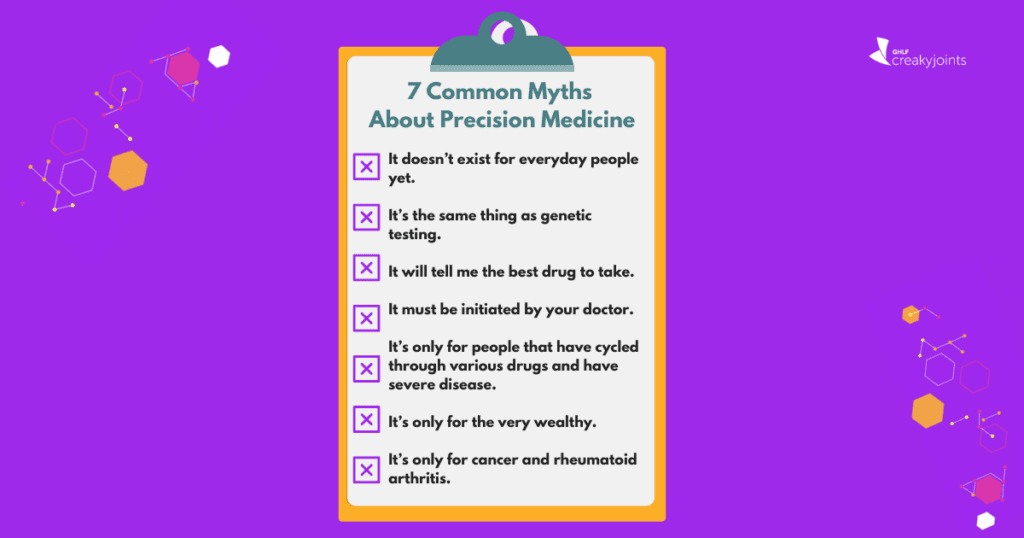
Here are seven common myths about precision medicine — and the real facts you need to know.
Myth 1: It doesn’t exist for everyday people yet.
There are commercially available tools that can help you and your doctor get started with precision medicine right away, including PrismRA. This is a blood test that determines if you’re unlikely to respond to TNFi medications, a common treatment route.
When patients with moderate to severely active disease were prescribed treatment based on their PrismRA result, they saw clinical improvements that were three times higher than those whose treatment didn’t align with test results, per a 2021 study in the journal Expert Review of Molecular Diagnostics funded by Scipher Medicine Corporation (the manufacturer of PrismRA).
Another available precision medicine tool is Vectra, which measures your rheumatoid arthritis inflammation and predicts your risk of radiographic progression by measuring 12 biomarkers — and incorporating that information with data on your age, gender, and more.
Tools like this aren’t very widely known yet. In a Global Healthy Living Foundation survey, as much as 70.9 percent of participants did not know what precision medicine is — and 26.6 percent knew about it but had never used it. However, after reading a description of precision medicine, most participants reported it would be very useful (59.8 percent) or somewhat useful (25.7 percent) in achieving their rheumatoid arthritis treatment goals.
A patient, who preferred to remain anonymous, was interviewed by CreakyJoints after undergoing precision medicine testing. She only heard about it from her own research and patient groups — not her doctor (though she reviewed the results with her rheumatologist). “The PrismRA test showed that I had a less than 10 percent chance of responding to any TNF inhibitor,” she says. “It was incredibly useful to me because I would have kept trying TNF inhibitors without it.”
Myth 2: It’s the same thing as genetic testing.
Precision medicine for conditions like rheumatology actually involves a combination of genetic testing, molecular profiling, and other diagnostic assessments.
“It’s all of that put together,” says Grace Wright, MD, a consultant rheumatologist in New York City and President of the Association of Women in Rheumatology. “I need to know what your blood tells me in terms of inflammatory markers, if you have markers for more severe disease, and the biomarker composite that we see in a test like PrismRA.”
Your doctor might also look at imaging studies to determine if your X-rays show evidence of bone erosion, which would be indicative of more progressive and extensive disease.
In other words, genetic testing is just one component of precision medicine that helps to inform your individual health care decisions.
“A defining assertion of precision medicine is that genomics — no matter how powerful or economical — is far from sufficient to understand human physiology and pathophysiology,” note the authors of a 2015 editorial in Science Translational Medicine. “Other components — molecular, developmental, physiological, social, and environmental — also must be monitored, aligned, and integrated.”
Myth 3: It will tell me the best drug to take.
Precision medicine isn’t designed to tell you the exact drug that will work best for you, but it may tell you and your doctor which one you shouldn’t start with. This, in turn, could save you months of trial and error.
For instance, PrismRA provides you with data showing your probability of response to TNFi therapy. If your doctor is considering putting you on a TNFi but the test’s interpretation criteria shows that you only have a five percent chance of responding to TNFi, they’ll likely try another drug first.
“My results said that I respond to TNF inhibitors, which makes sense because I always felt the best on them,” says Los Angeles-based Elaine Wiley, who has rheumatoid arthritis and scleroderma — and who took the PrismRA test. “Since my test, I’ve continued on my current B-cell therapy because it treats both of my autoimmune diseases. However, I think it’s extremely beneficial to know that if we’re able to work with the side effects, maybe we could go back to the TNF inhibitors.”
The results also aren’t an end-all for your treatment options. Your doctor will review all other aspects of your health as well.
“Rheumatoid arthritis is not just a joint disease; it’s a systemic disease,” says Dr. Wright. “When we look at the best course of therapy, I take into account heart health, lung health, and so forth. It’s important to understand why a treatment choice is being made, even if the test says we should start someplace else.”
When your treatment plan is determined based on your whole health picture and data from precision medicine, the results can be impactful. Of the survey participants who have used precision medicine testing, they reported that it was useful for making them feel more confident in the medications they take (34.5 percent), plan for the future (31.0 percent), and feel better faster (27.6 percent).
Myth 4: It must be initiated by your doctor.
With precision medicine, self-advocacy is key. Many doctors are still learning about precision medicine — and your rheumatologist may not be in the routine of bringing it up to patients.
Even though about half of GHLF survey participants who use precision medicine found it useful, only 2.6 percent of total participants reported their doctor using it to find a treatment that may work better for managing their rheumatoid arthritis.
However, of the participants who did not know what precision medicine was or had never used it, 42.9 percent said that they were very likely and 28.6 percent said they were somewhat likely to ask their doctor about it in the future after they had learned about it.
“Don’t be scared to approach your physician or your rheumatologist about asking for these tests,” says Wiley. “I have more often encountered a physician who is open to my questions about things I’ve researched than one who is put off about it.”
Even if your doctor does bring it up, make sure your questions are answered during your appointment. Of those who had used precision medicine in the survey, about a third only discussed the testing or results with their doctor once (31 percent), while another third discussed it at most appointments (31 percent). More than a third reported spending one to two minutes discussing precision medicine during their appointment (34.5 percent) while 27.6 percent reported spending a quarter of the appointment on the topic.
If you’re open to it, you can also ask about opportunities to join research for precision medicine. “Right now, we need to talk to our patient base and say let’s work as a team to treat this disease,” says Harris Perlman, PhD, Chief of Rheumatology at Northwestern University Feinberg School of Medicine. “The only way to do it is if you join our research projects.”
For instance, many centers working on precision medicine and rheumatology are looking for people willing to undergo synovial biopsies, says Dr. Perlman, who is personally involved in studies that perform those biopsies. In synovial biopsies, tissue samples from the lining of your joint are extracted for analysis to learn more about the mechanisms of your disease — another form of precision medicine.
Myth 5: It’s only for severe cases after trying multiple drugs.
A test like PrismRA is typically recommended for those who haven’t tried a biologic treatment yet. So, if you’ve tried methotrexate but it isn’t working and you need to escalate, the test could inform you of the next treatment decision.
“You want to make sure that, if at all possible, you can get a precise start to your treatment journey,” says Dr. Wright. “I think this myth partly comes from the fact that this is a relatively new thing, and for many patients, they’ve already cycled through six or seven drugs — so they’re getting this at the later stage of their journey.”
However, that doesn’t mean that’s the optimal treatment course. You don’t have to wait until the very end of your treatment journey, and in fact, it’s likely best employed in the beginning.
“The sooner we get your disease under control, the better your outcome is and the less likely you are to have damage and progression,” says Dr. Wright.
To that point, don’t believe the myth that precision medicine is only for severe cases of rheumatic diseases. Ideally, it’s a proactive approach that intervenes early on in your disease to prevent progression with the right treatment plan.
“Whether you’re coming in with very severe or moderate disease, you’re still capable of having a precision medicine approach,” says Dr. Wright.
Myth 6: It’s only for the very wealthy.
Your insurance may cover precision medicine, making it an affordable option for you (and less pricey than cycling ineffective drugs). For instance, Medicare covers PrismRA and most patients tested pay less than $75.
“For those who are on commercial, non-federal plans, it depends on the contract,” says Dr. Wright. “But in many cases, there is patient assistance support to help manage and offset the copay for these tests.” The patient interviewed by GHLF noted that although her insurance didn’t cover the test, the company that made the test told her they would dispute it so she wouldn’t be charged more than $75 — and so far, she hasn’t received a bill.
Myth 7: It’s only for cancer and rheumatoid arthritis.
Precision medicine can be used for anything from cancer to heart disease, obesity, osteoporosis, and diabetes, per the U.S. Centers for Disease Control and Prevention.
However, people may often think of precision medicine in terms of rheumatoid arthritis and cancer because there are so many different therapeutics to choose from in these diseases. “For other diseases, like vasculitis or scleroderma, there are fewer therapeutics,” says Dr. Perlman.
That said, advancements are on the horizon for other rheumatic conditions. “While precision medicine is still in its infancy in rheumatic disease, advancements in molecular profiling technologies and stratification techniques gives hope for new therapeutic options and personalized treatments in SARDs [systemic autoimmune rheumatic diseases],” note the authors of a 2022 review in Nature Medicine.
These SARDs include lupus and systemic sclerosis.
“Precision medicine is evolving in fields like lupus,” says Dr. Wright. “But we won’t use all the same tests for all our immune-mediated inflammatory diseases. It’s really important to know what your diagnosis is and what precision medicine tools are available for your disease.”
This article is part of “Your Guide to Precision and Personalized Medicine for Rheumatoid Arthritis” and was made possible with support from Scipher Medicine.
Listen: Understanding Precision and Personalized Medicine for Rheumatoid Arthritis
The Promise of Precision Medicine. National Institutes of Health. November 16, 2023. https://www.nih.gov/about-nih/what-we-do/nih-turning-discovery-into-health/promise-precision-medicine.
Strand V, et al. Clinical utility of therapy selection informed by predicted nonresponse to tumor necrosis factor-ɑ inhibitors: an analysis from the Study to Accelerate Information of Molecular Signatures (AIMS) in rheumatoid arthritis. Expert Review of Molecular Diagnostics. December 30, 2021. doi: https://doi.org/10.1080/14737159.2022.2020648.
Interview with Grace Wright, MD, a consultant rheumatologist in New York City and President of the Association of Women in Rheumatology
Hawgood S, et al. Precision medicine: Beyond the inflection point. Science Translational Medicine. August 12, 2015. doi: https://doi.org/10.1126/scitranslmed.aaa9970.
Interview with Harris Perlman, PhD, Chief of Rheumatology at Northwestern University Feinberg School of Medicine
Precision health: Improving health for each of us and all of us. Genomics & Precision Health. U.S. Centers for Disease Control and Prevention. May 17, 2022. https://www.cdc.gov/genomics/about/precision_med.htm.
Guthridge JM, et al. The promise of precision medicine in rheumatology. Nature Medicine. July 4, 2022. doi: https://doi.org/10.1038/s41591-022-01880-6.