Check out “Your Guide to Precision and Personalized Medicine for Rheumatoid Arthritis” for more information on this topic.
For many people living with rheumatoid arthritis (RA), finding the right treatment can pose significant challenges. Often, they must endure a trial-and-error process, waiting for months to gauge whether a medication is effective for them.
However, there’s hope of reducing this process with precision medicine. This innovative approach personalizes medical interventions to the unique characteristics of each patient, steering away from the outdated notion of ‘one-size-fits-all’ treatments. By considering factors like genetics, precision medicine aims to pinpoint the most effective treatment strategies for patients.
While precision medicine has seen popularity in oncology, its integration into rheumatology has been more limited. The good news is that there are precision medicine tests gaining traction, such as PrismRA, which is a blood test that assesses the likelihood of a person responding to TNF treatment.
To shed light on the perspectives of our RA community regarding precision medicine, flares, and remission, we conducted a survey in June-July 2022. We learned that the majority (94 percent) were not having conversations with their rheumatologist about precision medicine.
Now, a little over a year later we wanted to learn more about our community’s experience with precision medicine — if they’ve tried it, and how they believe it may help with their treatment plan.
To learn more, CreakyJoints conducted an online survey of 1,130 members with a diagnosis of RA. Participants were an average age of 63, majority were female (89 percent), most identified as white (86 percent), and the average time since diagnosis was 13 years.
Participants were asked questions on a range of topics, including:
- Duration of diagnosis
- Medication history
- Treatment objectives
- Awareness and application of precision medicine
- Concerns regarding insurance
- Interest in future applications of precision medicine
What We Asked
We wanted to understand a few general areas:
- Have people with rheumatoid arthritis used precision medicine?
- The usefulness of precision medicine testing between participants who have used it and those who have not.
- Participants’ goals for rheumatoid arthritis treatment.
What We Learned
1. There is an awareness gap when it comes to precision medicine and rheumatoid arthritis but patients do want to learn more and see the benefits.
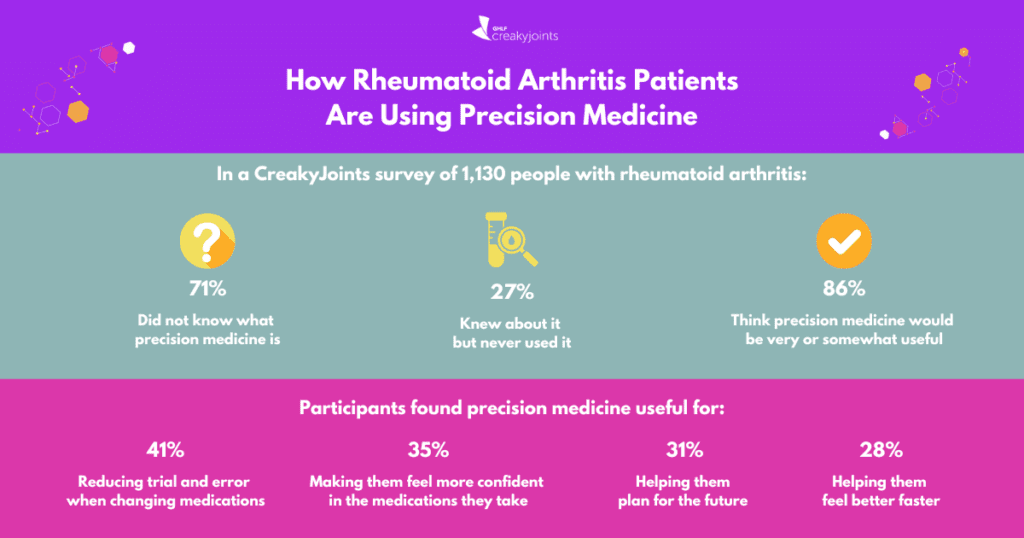
A whopping 71 percent of participants confessed to being in the dark about what precision medicine actually entails. This glaring awareness gap underscores the urgent need to educate patients.
Despite this lack of awareness, our findings revealed an intriguing desire among rheumatoid arthritis patients to learn more about precision medicine and its potential benefits. Even without a clear understanding, patients still want to learn about it and agree it could be helpful.
What’s particularly striking is the similarities between participants who were considering using precision medicine as part of their treatment and those who had already used precision medicine, especially concerning their desired outcomes, such as:
- Reducing trial and error when changing medications (68 percent)
- Helping them feel better faster (64 percent)
- Making them feel more in control of their disease (64 percent)
- Making them feel more confident in the medications they take (53 percent)
These participants reported that they were very likely (43 percent) or somewhat likely (29 percent) to ask their doctor about precision medicine in the future.
2. There is limited utilization of precision medicine among those with RA.
Only a small percentage of participants (2.6 percent) reported using precision medicine in their RA treatment journey. About a third reported using the PrismRA blood test (31 percent), another third reported using Vectra (31 percent), and another third reported not knowing which test was used (34.5 percent). This suggests a disconnect between the availability of precision medicine and its uptake among patients.
3. Whether or not they’ve used precision medicine, the majority of RA patients agree it is/would be helpful.
About half of participants who have used precision medicine testing found it useful (52 percent) while about a quarter reported that it was not (24 percent).
They reported that it was useful for:
- Reducing trial and error when changing medications (41 percent)
- Making them feel more confident in the medications they take (35 percent)
- Helping them plan for the future (31 precent)
- Helping them feel better faster (28 percent)
For the portion of respondents who didn’t know about it or never used it, most participants reported precision medicine would be very useful (60 percent) or somewhat useful (26 percent) in achieving their RA treatment goals after reading a description of what precision medicine is.
4. Common factors that play into treatment decisions include side effects, insurance coverage, and past treatments.
When asked what is important to them in deciding whether to switch medications, participants reported the following:
- Side effects (83 percent)
- Insurance coverage (67 percent)
- Past treatments (41 percent)
- Other conditions besides RA (38 percent)
What This Tells Us
This survey highlights a gap in understanding among many people with RA regarding precision medicine and its potential benefits. Despite a desire for symptom relief and improved well-being, precision medicine isn’t widely utilized in their treatment. It suggests a need for better patient education on the topic and increased discussion between doctors and patients. Encouragingly, many participants expressed interest in precision medicine, offering an opportunity to incorporate it more effectively in RA treatment. This could help shorten the trial-and-error process and have patients responding to treatment sooner.
This article is part of “Your Guide to Precision and Personalized Medicine for Rheumatoid Arthritis” and was made possible with support from Scipher Medicine.
Listen: Shilpa’s Rheumatoid Arthritis Journey
CreakyJoints Survey: Precision Medicine Needs Assessment. November 2023.