Everyone knows that rheumatoid arthritis attacks the joints, so of course it causes joint pain, stiffness, and swelling. And sure, all that inflammation inside your body can lead to major-league fatigue. But for some people, that’s the half of it.
“About 40 percent of people with RA have non-joint symptoms that can affect everything from the lungs and eyes to the cardiovascular system,” says Emily Carroll, MD, an internist focusing on rheumatological diseases at New York’s Mount Sinai Hospital. “RA is a systemic autoimmune phenomenon; that same autoimmune phenomenon can happen throughout the body.”
What’s more, she says, it’s important to be attuned to those lesser-known symptoms and act on them. “When in doubt, it never hurts to reach out to your rheumatologist and let them know. We don’t want people to sit on a symptom,” says Dr. Carroll. “Often, if we pick it up sooner, we can prevent damage.”
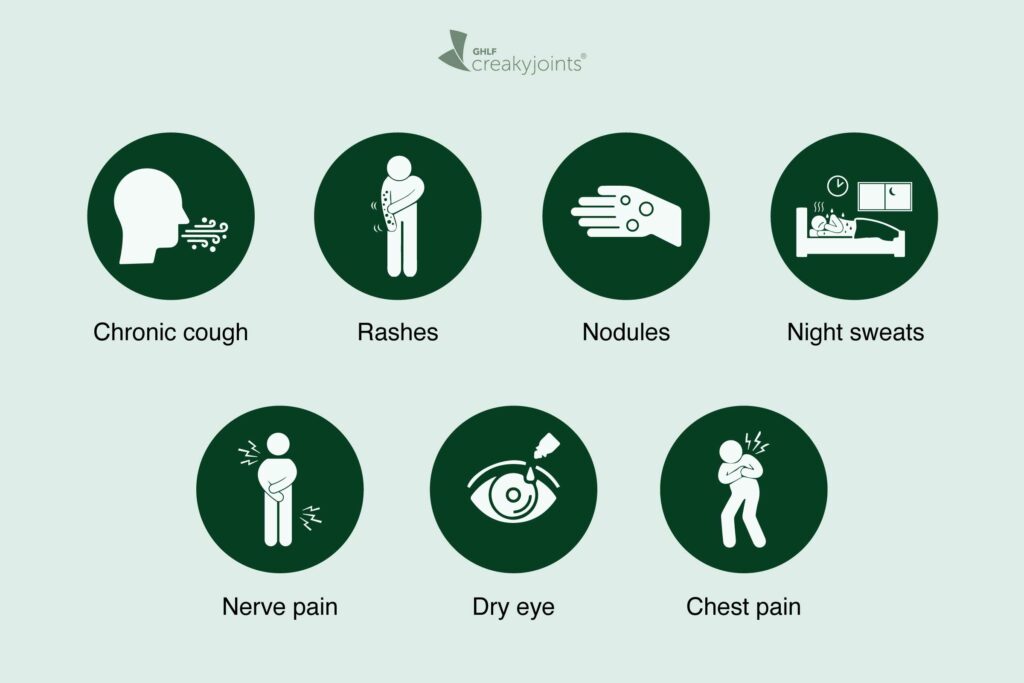
7 Symptoms of Rheumatoid Arthritis We Don’t Talk About
Here’s a closer look at some of the RA symptoms that can fly under the radar and what you should know about them.
Chronic Cough
“One of the biggest non-joint areas we pay close attention to is the lungs,” says Dr. Carroll. Inflammation in the lungs can show up with a chronic cough or feeling shortness of breath during ordinary activity. It can be quite serious, leading to nodule formation and scarring within the lungs, she adds, so alert your doctor if you experience cough or shortness of breath. You may be a candidate for a biologic or biosimilar medication if you’re not using one already.
Rashes, Bruising, and Discoloration
RA can cause rheumatoid vasculitis (RV), inflammation of the blood vessels. “That can be the reason for rashes and discoloration you can see on the skin,” explains Dr. Carroll. It can also cause sores and redness around the fingertips and fingernails.
Marilyn Gomez, a Modesto, CA-based astrologer and business coach who has been living with RA since she was 9 years old, not only noticed that her skin was thinning but that “bluish, purplish lines were starting to form.”
Like Marilyn, most people who get RV have had RA for a long time and often have severe joint deformities. Marilyn had all the bones in her toes broken and reset because the deformities in her feet were so excruciating — she said it felt like she was “walking on rocks.” Depending on how bad your RV is, treatment can include immunosuppressants, such as methotrexate, or biologics or biosimilars.
Nodules
People with RA can also develop lumps or nodules near joints that get lots of use. “For instance, if you kneel a lot for your job, they might appear on your knees,” says Dr. Carroll. Or if you lean on your elbows, they might form there. Ranging from the size of a pea to that of a lemon, nodules are not serious and usually don’t hurt — in fact, they often go away on their own.
However, if they’re bothering you, a corticosteroid injection can help shrink them. Perhaps the most important thing to know about nodules is that they’re a marker of more serious disease, meaning your RA is not well controlled. If you develop nodules, it’s an opportunity to talk about treatment options with your rheumatologist.
Night Sweats
“When I’m in a flare, I feel like I have the flu all over,” says RA patient advocate Eileen Davidson, who lives in Vancouver, Canada. “I wake up with full-body night sweats. Some days if they’re really bad, they can soak through the bedding.”
For Palm Springs, CA-based fashion designer Michael Kuluva, night sweats were a regular occurrence for a couple years: “I would wake up shivering and covered head to toe in sweat. When I would get out of bed to switch clothing, I could see the entire outline of my body in the sheets.”
Dr. Carroll says night sweats and fevers can be symptoms of immune system activation; however, the better you control the disease, the less likely these things are to happen. And suddenly experiencing a night sweat out of nowhere should be looked into. “It could be potentially related to an infection,” says Dr. Carroll. “Bring it up to your doctor so you can rule out anything serious.”
Nerve Pain and Tingling
Inflammation and bone erosion in the wrists and ankles can affect the nerves traveling through the joints, while inflammation at the very top of the cervical spine can also compress the nerves, causing neck pain, explains Dr. Carroll.
For Marilyn, it manifested as tingling sensations and shooting nerve pain down the sides of her feet and hands near the pinkies. Wearing braces at night and a hand stabilizer during the day has helped, says Marilyn, who also notes less nerve pain since starting a biologic 14 years ago.
Dry Eye
“And it’s round-the-clock dry eye,” says Marilyn. “I can’t wear contacts, because it’s too irritating.” In some people with RA, the same antibodies that attack the joints can inhibit tear production. Dr. Carroll says red, painful irritated eyes should be brought to the attention of your rheumatologist because it can be vision threatening if untreated.
To combat the dryness and itchiness, Marilyn always carries lubricating drops and sees her ophthalmologist for regular visits; however, some people may need to supplement with steroid drops or might need biologics, says Dr. Carroll.
Sharp Chest Pain
RA can lead to pericarditis, an inflammation of the membrane surrounding the heart. “The classic symptom is people get this sharp pain in their chest especially when taking a deep breath, coughing, or when lying flat,” says Dr. Carroll. It’s usually not serious and can be managed with medication, but that doesn’t mean you should assume any sharp chest pain is pericarditis.
In fact, it’s a good idea to call your health care professional or 911 to rule out a heart attack or other cardiovascular event if you feel chest discomfort. As Dr. Carroll points out, “People with RA are at high risk for early heart disease. For one, inflammation is a big driver of plaque formation [cholesterol buildup]. Also, when your joints hurt, it’s hard to move, so you may be prone to weight gain.”
Not Sure What’s Causing Your Pain?
Check out PainSpot, our pain locator tool. Answer a few simple questions about what hurts and discover possible conditions that could be causing it. Start your PainSpot quiz.